- Visibility 180 Views
- Downloads 44 Downloads
- Permissions
- DOI 10.18231/j.aprd.2025.010
-
CrossMark
- Citation
Comparative analysis of accuracy of SLA and DMLS technologies for cast partial denture frameworks using metrology software
Abstract
Introduction: Advanced manufacturing techniques like CAD/CAM and 3D printing have revolutionized dental prosthetics, offering improved precision, efficiency, and accessibility. The accuracy and precision of cast partial dentures significantly affect patient outcomes.
Aims and Objectives: To compare the trueness and precision of stereolithography (SLA) and Direct Metal Laser Sintering (DMLS) in fabricating Cast Partial Denture (CPD) frameworks.
Materials and Methods: A partially edentulous mandibular replica was scanned to create a master STL file. Using CAD software, 32 frameworks were designed and produced: 16 using DMLS and 16 using SLA. The frameworks were digitized using a high-precision scanner and compared to the original CAD design using 3D analysis software. Five Areas of Interest (AOIs) were identified: the lingual plate, right and left I-bars, and right and left proximal plates. Gap distances and Root Mean Square (RMS) values were calculated for statistical analysis.
Results: No statistically significant differences were found between DMLS and SLA techniques across the five AOIs (p > 0.05). RMS values for DMLS ranged from 0.0290 mm to 0.0348 mm, whereas SLA values ranged from 0.0337 mm to 0.0387 mm. The right proximal plate showed a marginally non-significant difference (p = 0.0560), favoring DMLS.
Conclusion: Both DMLS and SLA techniques demonstrated comparable accuracy in producing cast partial denture frameworks across all examined areas. This study provides valuable insights for dental professionals in selecting manufacturing techniques for CPD frameworks by considering factors such as cost and material properties.
Introduction
The prognosis of patients with partially edentulous arches can be greatly influenced by the accuracy and precision of the cast partial dentures. Several elements can affect the fit and precision of cast partial denture frameworks, including impression type and intraoral scanning head dimensions, [1] quantity and position of absent teeth, [2] and technology used in framework production. [3]
The field of dentistry has been transformed by the introduction of cutting-edge manufacturing techniques that have dramatically enhanced patient outcomes and the creation of dental prostheses. The development of computer-aided design and computer-aided manufacturing (CAD/CAM) systems has enabled the production of highly accurate and personalized dental implants, crowns, bridges, and cast partial dentures, offering unprecedented levels of precision and fit. [4] These digital workflows allow dental professionals to design prostheses with exceptional details, considering individual patient anatomy and bite relationships.
The potential of dental prosthetics has been further expanded by 3D printing, which enables the swift prototyping of intricate dental structures with complex geometries that were previously difficult or impossible to create using conventional methods. [5] This additive manufacturing approach allows for the direct production of patient-specific implants, surgical guides, and even temporary prostheses in dental offices, thus reducing the need for multiple patient visits and improving treatment efficiency.
These advanced technologies not only improve fit accuracy, but also substantially decrease production time and expenses, making high-quality dental prostheses more accessible to a wider range of patients. The digital nature of these processes also facilitates improved communication among dentists, laboratories, and patients, allowing for more collaborative treatment planning and predictable outcomes. [6]
Assessing the precision of cutting-edge manufacturing methods in dental prosthetics is essential to guarantee optimal performance, visual appeal, and patient satisfaction. This assessment encompasses various critical factors including dimensional precision, fit evaluation, surface quality, material durability, and biocompatibility. [7]
Innovative manufacturing techniques such as stereolithography (SLA) and Direct Metal Laser Sintering (DMLS) have transformed the production of dental prostheses. These technologies provide notable benefits in terms of accuracy, personalization, and productivity. SLA is an additive manufacturing method that employs a laser to harden liquid resin in a layer-by-layer process. [8] This approach is particularly beneficial in creating intricate dental models, surgical guides, and temporary prostheses. SLA has been used to produce provisional crowns and trial dentures with varying levels of accuracy. For provisional crowns, SLA demonstrated lower trueness and precision than subtractive methods. [9] In the case of trial dentures, the SLA achieved trueness ranging from 22.5 to 49.6 μm and precision between 18.7 and 26.9 μm, contingent on the measured surface. [9] The thickness of the layers in SLA can influence the accuracy, with 100 μm layers yielding superior results compared to 50 μm for trial dentures. [10]
In contrast, DMLS utilizes a powerful laser to sinter metal powder particles and merge them into a solid structure. [11] DMLS enables the creation of intricate geometries with high strength and longevity. RPD frameworks fabricated using DMLS generally exhibit higher trueness and precision than those fabricated using conventional casting methods. [12] Some studies indicate that precision casting outperforms DMLS technology when comparing the adaptation of frameworks with extensive spans, including more retainers and clasps. [13]
The current research landscape lacks comprehensive studies comparing the trueness and precision of Stereolithography (SLA) and Direct Metal Laser Sintering (DMLS) in the production of cast partial denture frameworks. This study aims to address this knowledge gap by quantitatively evaluating the accuracy of stereolithography (SLA) and Direct Metal Laser Sintering (DMLS) in the fabrication of Cast Partial Denture (CPD) frameworks.
Materials and Methods
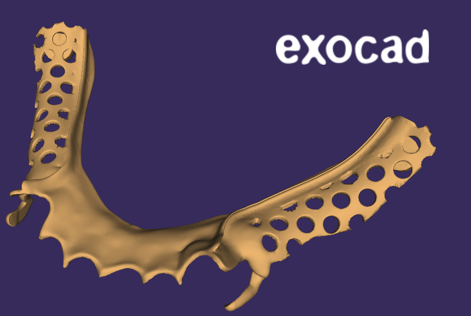
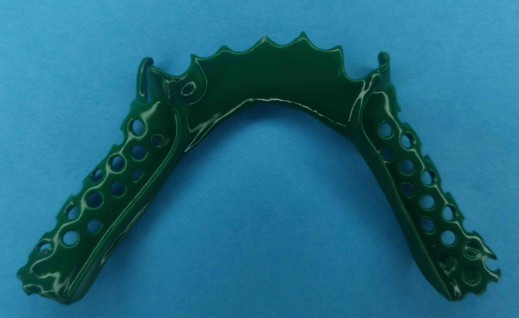
A simulation model using a partially edentulous mandibular replica was employed. The distal proximal surfaces of both canines were prepared using the guide planes. A high-resolution scanner (inEos X5; Dentsply Sirona) was used to scan the model and generate a master STL file. This file was then imported into the CAD software Exocad (version 3.1, Exocad GmbH, Darmstadt, Germany) to create a detailed mandibular removable partial denture (RPD) framework design as shown in [Figure 1], which included key elements such as the major connector, clasps, and rest. Subsequently, 32 frameworks were produced: 16 using Direct Metal Laser Sintering (DMLS) technology (Cobalt-Chromium-Molybdenum super alloy powder) as shown in [Figure 4] and 16 using stereolithography (SLA) 3D printing as shown in [Figure 3] (Elegoo Dental Castable Resin). To ensure consistency and eliminate design-related variables, all 32 frameworks were fabricated using identical digital design files. This method enabled a direct comparison between the two manufacturing techniques, while maintaining design uniformity across all samples.
To preserve the original characteristics of the cast partial frameworks and conduct an accurate analysis of their as-fabricated properties, post-production polishing or trimming was not performed. This approach maintained the initial surface features and dimensional precision of the frameworks. By refraining from any post-fabrication alterations, this study aims to evaluate the authentic performance and fit of the frameworks in their original state, reflecting the quality of the manufacturing process itself.
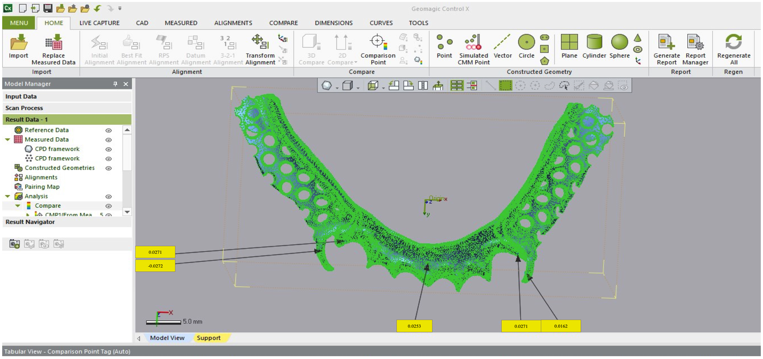
Digital acquisition and analysis of the 32 frameworks involved several critical steps to ensure an accurate comparison between the manufactured samples and their original CAD designs. All frameworks were digitized using a high-precision laboratory scanner with consistent scanning and positioning parameters. The resulting STL files were then imported into the specialized 3D analysis software Geomagic Control X software (version 2022.1.0.70, 3D Systems, Rock Hill, South Carolina, USA) as shown in [Figure 2]. These files were aligned with the corresponding master CAD design using best-fit algorithms.
The study identified three key Areas of Interest: the main connector (lingual plate), retentive portion of the I bar, and proximal plates on both sides. These areas were chosen because of their crucial role and potential influence on the overall effectiveness of the cast partial denture framework. The lingual plate, which served as the primary connector, was evaluated for its fit and stability along the lingual aspect of the mandibular arch. The retentive part of the I-bar was included to evaluate its efficacy in securing the dentures. The proximal plates on each side were selected to assess their adaptation to neighboring teeth and their contribution to denture stability. The sample distribution among various areas of interest have been depicted in [Table 1].
Geomagic software was used to superimpose and measure the original CAD design (reference model) against the scanned STL files of each produced framework. A local best-fit alignment was conducted focusing on the areas of interest. For each Area of Interest (AOI), the corresponding region was chosen for both the reference model and scanned framework. Software comparison tools were used to calculate the normal gap distance between the reference and manufactured surfaces at each sampling point. Deviation visualization was achieved by extracting the numerical data for statistical analysis. Gap distances were used to compute the Root Mean Square (RMS) values, which were then exported for statistical analysis.
After gathering data for both the DMLS and SLA groups, a thorough statistical analysis was performed using the SPSS software (version 26.0, IBM Corp., Armonk, NY, USA), with significance set at p < 0.05. Paired t-tests were used to compare gap distances between the DMLS and SLA groups.
Results
This study conducted a comprehensive analysis of dental prosthetic components produced using two different manufacturing methods: Direct Metal Laser Sintering (DMLS) and stereolithography (SLA). The results were analyzed across five Areas of Interest (AOI) using gap distance measurements and Root Mean Square (RMS) values, as shown in [Table 1].

|
AOI |
Designated area on Framework |
Samples (N) |
|
|
DMLS CPD Framework |
SLA CPD Framework |
||
|
AOI 1 |
Lingual Plate |
16 |
16 |
|
AOI 2 |
I-bar Right side |
16 |
16 |
|
AOI 3 |
I-bar Left side |
16 |
16 |
|
AOI 4 |
Proximal Plate Right side |
16 |
16 |
|
AOI 5 |
Proximal Plate Left side |
16 |
16 |
|
S.No. |
DMLS Gap Distance (mm) |
Mean RMS value of DMLS |
SLA Gap Distance (mm) |
Mean RMS value of SLA |
t-value |
p-value |
|
1 |
0.0253 |
0.0348 |
0.0342 |
0.0377 |
-0.6108 |
0.5505 |
|
2 |
0.0417 |
0.0385 |
||||
|
3 |
-0.0295 |
0.0613 |
||||
|
4 |
0.0311 |
-0.0436 |
||||
|
5 |
0.0356 |
0.0480 |
||||
|
6 |
0.0360 |
0.0401 |
||||
|
7 |
-0.0206 |
-0.0305 |
||||
|
8 |
0.0323 |
0.0305 |
||||
|
9 |
0.0386 |
0.0308 |
||||
|
10 |
0.0598 |
0.0433 |
||||
|
11 |
-0.0389 |
0.0324 |
||||
|
12 |
0.0316 |
0.0210 |
||||
|
13 |
-0.027 |
0.0280 |
||||
|
14 |
0.0313 |
-0.0338 |
||||
|
15 |
-0.0239 |
0.0272 |
||||
|
16 |
0.0465 |
-0.0355 |
|
S.No. |
DMLS Gap Distance (mm) |
Mean RMS value of DMLS |
SLA Gap Distance (mm) |
Mean RMS value of SLA |
t-value |
p-value |
|
1 |
0.0162 |
0.0340 |
0.0215 |
0.0387 |
0.8340 |
0.4173 |
|
2 |
0.0345 |
-0.0427 |
||||
|
3 |
0.0174 |
0.0454 |
||||
|
4 |
-0.0429 |
0.0342 |
||||
|
5 |
-0.021 |
0.0447 |
||||
|
6 |
0.0423 |
-0.0526 |
||||
|
7 |
0.0253 |
0.0391 |
||||
|
8 |
-0.0377 |
0.0430 |
||||
|
9 |
0.0411 |
0.0397 |
||||
|
10 |
0.0270 |
-0.0172 |
||||
|
11 |
-0.0365 |
0.0286 |
||||
|
12 |
0.0312 |
0.0510 |
||||
|
13 |
-0.0424 |
-0.0403 |
||||
|
14 |
0.0314 |
0.0389 |
||||
|
15 |
-0.0446 |
-0.021 |
||||
|
16 |
0.0526 |
0.0331 |
|
S.No. |
DMLS Gap Distance (mm) |
Mean RMS value of DMLS |
SLA Gap Distance (mm) |
Mean RMS value of SLA |
t-value |
p-value |
|
1 |
-0.0272 |
0.0290 |
0.0383 |
0.0337 |
-1.3463 |
0.1982 |
|
2 |
0.0236 |
-0.0393 |
||||
|
3 |
0.0380 |
0.0303 |
||||
|
4 |
0.0176 |
-0.0339 |
||||
|
5 |
0.0371 |
0.0206 |
||||
|
6 |
-0.0289 |
-0.048 |
||||
|
7 |
0.0307 |
0.0398 |
||||
|
8 |
-0.0234 |
0.0270 |
||||
|
9 |
-0.0265 |
0.0217 |
||||
|
10 |
0.0156 |
-0.0278 |
||||
|
11 |
0.0441 |
-0.0406 |
||||
|
12 |
-0.0332 |
0.0394 |
||||
|
13 |
0.0296 |
0.0316 |
||||
|
14 |
-0.0281 |
-0.0445 |
||||
|
15 |
0.0183 |
0.0345 |
||||
|
16 |
0.0240 |
0.0175 |
|
S.No. |
DMLS Gap Distance (mm) |
Mean RMS value of DMLS |
SLA Gap Distance (mm) |
Mean RMS value of SLA |
t-value |
p-value |
|
1 |
0.0271 |
0.0316 |
0.0317 |
0.0372 |
-2.0710 |
0.0560 |
|
2 |
-0.0303 |
-0.0347 |
||||
|
3 |
0.0341 |
0.0227 |
||||
|
4 |
-0.0212 |
0.0402 |
||||
|
5 |
-0.0459 |
0.0447 |
||||
|
6 |
-0.0205 |
-0.0497 |
||||
|
7 |
0.0448 |
0.0403 |
||||
|
8 |
0.0396 |
0.0325 |
||||
|
9 |
-0.0214 |
-0.0418 |
||||
|
10 |
0.0299 |
0.0342 |
||||
|
11 |
0.0333 |
0.0362 |
||||
|
12 |
0.0281 |
0.0514 |
||||
|
13 |
0.0345 |
-0.0242 |
||||
|
14 |
0.0341 |
0.0366 |
||||
|
15 |
-0.0184 |
0.0328 |
||||
|
16 |
0.0410 |
-0.0332 |
|
S.No. |
DMLS Gap Distance (mm) |
Mean RMS value of DMLS |
SLA Gap Distance (mm) |
Mean RMS value of SLA |
t-value |
p-value |
|
1 |
0.0271 |
0.0316 |
0.0317 |
0.0372 |
-1.6404 |
0.1217 |
|
2 |
-0.0303 |
0.0347 |
||||
|
3 |
0.0341 |
-0.0227 |
||||
|
4 |
0.0212 |
-0.0402 |
||||
|
5 |
-0.0459 |
0.0447 |
||||
|
6 |
0.0205 |
-0.0497 |
||||
|
7 |
-0.0448 |
0.0403 |
||||
|
8 |
0.0396 |
0.0325 |
||||
|
9 |
0.0214 |
0.0418 |
||||
|
10 |
0.0299 |
0.0342 |
||||
|
11 |
0.0333 |
0.0362 |
||||
|
12 |
0.0281 |
0.0514 |
||||
|
13 |
0.0345 |
0.0242 |
||||
|
14 |
-0.0341 |
-0.0366 |
||||
|
15 |
0.0184 |
0.0328 |
||||
|
16 |
0.0410 |
0.0332 |
For the lingual plate (AOI 1), as shown in [Table 2], the comparison between the DMLS and SLA techniques showed no significant difference (p = 0.5505). The RMS value for the DMLS technique was 0.0348 mm, whereas that for the SLA technique was 0.0377 mm. This suggests that both techniques performed similarly in terms of accuracy of the major connector area.
In the analysis of the right I-bar (AOI 2), as shown in [Table 3], the results again showed no statistically significant difference between the DMLS and SLA techniques (P = 0.4173). The RMS value of the DMLS technique was 0.0340 mm, whereas of that the SLA technique was 0.0387 mm. This indicates that both techniques provide comparable accuracy in manufacturing the retentive part of the I-bar on the right side.
For the left I-bar (AOI 3), as shown in [Table 4], there was no statistically significant difference between the two techniques (P = 0.1982). The RMS value for the DMLS technique was 0.0290 mm, whereas for that the SLA technique was 0.0337 mm. This suggests that both techniques perform similarly in terms of accuracy for the left I-bar, mirroring the results from the right side.
Analysis of the right proximal plate (AOI 4), as shown in [Table 5], revealed a marginally non-significant difference between the DMLS and SLA techniques (P = 0.0560). The RMS value of the DMLS technique was 0.0316 mm, whereas of that the SLA technique was 0.0372 mm. This suggests a trend towards better accuracy with the DMLS technique for the right proximal plate, although the difference was not statistically significant.
For the left proximal plate (AOI 5), as indicated in [Table 6], there was no statistically significant difference between the two techniques (p = 0.1217). The DMLS technique had an RMS value of 0.0316 mm, identical to AOI 4, whereas the SLA technique showed an RMS value of 0.0372 mm. This indicates that both techniques provide comparable accuracy in manufacturing the left proximal plate.
The results demonstrated that both the DMLS and SLA techniques produced cast partial denture frameworks with comparable accuracy across all five Areas of Interest. Although there were slight variations in the RMS values between the techniques and across different AOIs, none of these differences reached statistical significance.
Discussion
The results of this comprehensive study comparing Direct Metal Laser Sintering (DMLS) and stereolithography (SLA) methods for creating cast partial denture frameworks offer crucial insights into the precision and accuracy of these manufacturing techniques. The study revealed no statistically significant variations between DMLS and SLA approaches across all five Areas of Interest (AOI), indicating that both methods can produce dental prosthetics with similar levels of accuracy.
A comprehensive review and meta-analysis explored how different manufacturing techniques affect the accuracy and internal fit of removable partial denture (RPD) frameworks. The findings suggested that computer-aided design and computer-aided manufacturing (CAD-CAM) approaches, including additive manufacturing and milling techniques, yielded results that were either comparable to or better than those of traditional fabrication methods. Several factors influencing accuracy were noted, including software errors, intraoral scanner effectiveness, and patient-specific variables. CAD-CAM methods have shown promising potential, offering benefits such as acceptable internal fit and high patient satisfaction. The superimposition technique has been emphasized as a thorough method for assessing overall internal fit. As costs decrease and more specialized RPD design software becomes available, the potential ease of producing accurate frameworks using CAD-CAM increases. [14]
Although DMLS technology provides significant benefits in dentistry, its cost remains a factor to consider. Although this technique enables the creation of intricate dental structures with high precision and reliability, the manufacturing expense of DMLS can be substantial because of the high cost of metal powders. [15] DMLS-produced Co-Cr dental alloys have demonstrated superior hardness compared to conventionally cast alloys, [16] which could potentially offset expenses through enhanced performance and durability. Although DMLS-produced alloys exhibit a higher occurrence of internal porosities, these porosities are more evenly distributed and have significantly smaller mean and total volumes than cast alloys. [17]
Castable resins used in stereolithography (SLA) have become popular for producing intricate molds and patterns in dental applications. These resins are formulated to burn out cleanly, leaving minimal ash, making them suitable for investment casting. [18] SLA technology offers enhanced precision and replicability compared with conventional wax-up techniques, as digital designs can be accurately reproduced. The process is more efficient and less time-consuming than manual wax-ups, potentially reducing the production expenses. Additionally, castable resins enable the creation of complex shapes that may be challenging to achieve using traditional methods, offering greater design flexibility. However, SLA has some drawbacks, including the upfront cost of the 3D printing equipment and software. Dental technicians may face a learning curve when transitioning from the traditional methods. The casting process still requires expertise to ensure proper resin burnout and complete mold filling. Some castable resins may produce more residue than wax, potentially impacting the final casting quality if not handled properly.
Both DMLS and SLA technologies exhibited similar accuracies across all Areas of Interest (AOIs), with no statistically significant differences observed between them for any AOI. Nevertheless, DMLS displayed slightly lower RMS values for most AOIs, indicating a tendency towards improved accuracy. In terms of investment, DMLS requires a higher initial outlay for equipment and materials, whereas SLA has a lower upfront cost but requires additional investment in casting equipment and processes.
Other factors to consider include material properties, design flexibility, post-processing requirements, and adaptation process for dental technicians. DMLS produces Co-Cr alloys with greater hardness than conventional casting, whereas SLA utilizes castable resins, with final properties dependent on the casting process. Both technologies allow intricate geometries and digital design replication. DMLS requires minimal postprocessing, whereas SLA requires a casting process that may influence the final quality. Dental technicians transitioning from traditional methods may require training in both the technologies.
Geomagic and similar metrology software can be effectively used for STL file superimposition analysis in the production of cast partial denture frameworks. This method enables the precise assessment of fit and accuracy in digital dentistry processes. Research has shown the effectiveness of Geomagic in analyzing removable partial denture (RPD) frameworks. One investigation, [19] utilized Geomagic Control X to evaluate the overall and marginal deviations of frameworks from a master STL file using the root mean square method, and concluded that non-metrology-grade freeware might offer comparable overall deviation measurements in certain cases. Another study used Geomagic Control X for digital superimposition and direct measurements to evaluate the RPD framework fit, finding it similar to high-resolution micro-computed tomography techniques. [20]
The quality of superimposition analysis can be influenced by the accuracy and resolution of the STL file-generating scanning process as well as the selection of reference points or areas for alignment during superimposition. [21] This study used an industrial scanner with high precision to main standardisation among the samples. Each STL file was exported to the superimposition software without compromising on quality.
The importance of this study lies in its thorough comparison of two advanced manufacturing methods for creating cast partial denture frameworks: Direct Metal Laser Sintering (DMLS) and stereolithography (SLA). This study fills a crucial gap in the existing literature by quantitatively assessing the accuracy of these technologies across multiple areas of interest in dental prosthetics. The results indicate that both DMLS and SLA can produce comparably accurate frameworks, challenging the notion of the superiority of one technique. This information is vital for dental professionals and laboratories to make informed decisions regarding technology adoption and investment. An in-depth analysis of specific areas (such as the lingual plate, I-bars, and proximal plates) offers valuable insights into the performance of these technologies in the critical functional areas of cast partial dentures. These findings have significant implications for enhancing the fit, comfort, and overall quality of dental prostheses, potentially leading to improved patient outcome and satisfaction.
Despite providing valuable insights into DMLS and SLA technologies for cast partial denture frameworks, this study had certain limitations. The small sample size may restrict the generalizability of our findings, necessitating further research with larger datasets. Post-SLA processing errors could have introduced unintended variations in the final products, potentially affecting the accuracy of measurements. The alteration of metrology software parameters during the analysis may have affected the measurement consistency across samples. The industrial scanner used for measurements, although highly accurate, still has inherent limitations that could influence the precision of the results. Furthermore, the absence of clinical data, such as framework fit and patient comfort, limits the ability of the study to draw conclusions about the real-world performance of these technologies in patient care scenarios. These limitations underscore the need for future studies to address these factors to provide a more comprehensive understanding of the clinical implications of DMLS and SLA technologies in dental prosthetics.
Conclusion
This study provides valuable evidence to support the use of both DMLS and SLA techniques in the production of dental prosthetic components. The comparable accuracies across various Areas of Interest suggest that both methods can reliably produce high-quality cast partial denture frameworks. However, further research is needed to explore the clinical implications of the subtle differences observed between these techniques and to investigate their performance in diverse patient populations and complex prosthetic designs.
Ethical Committee Approval
Obtained from the ethical committee.
Source of Funding
Self-funded.
Conflict of Interest
None.
Acknowledgement
I would like to thank the KLE VK Institute of Dental Sciences and Department of Prosthodontics for supporting me through the research project.
References
- Hayama H, Fueki K, Wadachi J, Wakabayashi N. Trueness and precision of digital impressions obtained using an intraoral scanner with different head size in the partially edentulous mandible. J Prosthodont Res. 2018;62(3):347-52. [Google Scholar]
- Lee J, Han J, Yeo I, Yoon H, Yun J. Repeatability of Intraoral Scanners for Complete Arch Scan of Partially Edentulous Dentitions: An In Vitro Study. J Clin Med. 2019;8(8). [Google Scholar] [Crossref]
- Almufleh B, Emami E, Alageel O, Melo F, Seng F, Caron E. Patient satisfaction with laser-sintered removable partial dentures: A crossover pilot clinical trial. J Prosthet Dent. 2017;119(4):560-7. [Google Scholar]
- Cevik P, Yilmaz B, Schimmel M. New generation CAD-CAM materials for implant-supported definitive frameworks fabricated by using subtractive technologies. Biomed Res Int. 2022. [Google Scholar] [Crossref]
- Rezaie F, Dahri M, Moharamzadeh K, Amini F, Wirth J, Masjedi M. 3D Printing of Dental Prostheses: Current and Emerging Applications. J Compos Sci. 2023;7(2). [Google Scholar] [Crossref]
- Pillai S, Wang Y, Tarar M, Lee K, Harb I, Zhou S. Dental 3D-Printing: Transferring Art from the Laboratories to the Clinics. Polymers. 2021;13(1). [Google Scholar] [Crossref]
- Fadzil A, Pramanik A, Basak A, Prakash C, Shankar S. Role of surface quality on biocompatibility of implants - A review. Ann 3D Printed Med. 2022;8. [Google Scholar] [Crossref]
- Espino M, Robles G, Dizon J, Tuazon B. Application of Taguchi Methodology in Evaluating the Rockwell Hardness of SLA 3D Printed Polymers. Mater Sci Forum. 2020;1005(2):166-73. [Google Scholar]
- Kang S, Kim J, Park J, Kim W. Accuracy of provisional crowns made using stereolithography apparatus and subtractive technique. J Adv Prosthodont. 2018;10(5):354-60. [Google Scholar]
- You S, You S, Kang S, Bae S, Kim J. Evaluation of the accuracy (trueness and precision) of a maxillary trial denture according to the layer thickness: An in vitro study. J Prosthet Dent. 2020;125(1):139-45. [Google Scholar]
- Moletsane M, Krakhmalev P, Kazantseva N, Plessis D, Yadroitsava A, I, et al. Tensile properties and microstructure of direct metal laser-sintered TI6AL4V (ELI) Alloy. South Afr J Ind Eng. 2016;27(3):110-21. [Google Scholar]
- Peng P, Hsu C, Huang H, Chao J, Lee W. Trueness of removable partial denture frameworks additively manufactured with selective laser melting. J Prosthet Dent. 2020;127(1):122-7. [Google Scholar]
- Chen H, Li H, Zhao Y, Zhang X, Wang Y, Lyu P. Adaptation of removable partial denture frameworks fabricated by selective laser melting. J Prosthet Dent. 2019;122(3):316-24. [Google Scholar]
- Rokhshad R, AT, Zarbakhsh A, Revilla-León M. Influence of fabrication method on the manufacturing accuracy and internal discrepancy of removable partial dentures: A systematic review and meta-analysis. J Prosthet Dent. 2023;S0022-3913(23). [Google Scholar] [Crossref]
- López-Castro J, Marchal A, González L, Botana J. Topological optimization and manufacturing by Direct Metal Laser Sintering of an aeronautical part in 15-5PH stainless steel. Procedia Manuf. 2017;13:818-24. [Google Scholar]
- Lapcevic A, Eggbeer D, Puskar T, Jevremovic D, Williams R. Comparative analysis of structure and hardness of cast and direct metal laser sintering produced Co-Cr alloys used for dental devices. Rapid Prototyping J. 2016;22(1):144-51. [Google Scholar]
- Schweiger J, Güth J, Erdelt K, Edelhoff D, Schubert O. Internal porosities, retentive force, and survival of cobalt-chromium alloy clasps fabricated by selective laser-sintering. J Prosthodont Res. 2019;64(2):210-6. [Google Scholar]
- Corcione CE, Greco A, Licciulli A, Maffezzoli A, Montagna F. Free form fabrication of silica moulds for aluminium casting by stereolithography. Rapid Prototyping J. 2006;12(4):184-8. [Google Scholar]
- Dede D, Çakmak G, Donmez M, Küçükekenci A, Lu W, Ni A. Effect of analysis software program on measured deviations in complete arch, implant-supported framework scans. J Prosthet Dent. 2023;132(1):211-8. [Google Scholar]
- Conceição P, Portugal J, Franco M, Alves N, Marques D, Neves C. Comparison between digital superimposition and microcomputed tomography methods of fit assessment of removable partial denture frameworks. J Prosthet Dent. 2023;131(3):479-86. [Google Scholar]
- Oh K, Yun B, Kim J. Accuracy of metal 3D printed frameworks for removable partial dentures evaluated by digital superimposition. Dent Mater. 2021;38(2):309-17. [Google Scholar]
How to Cite This Article
Vancouver
Swami RS, Doddamani MH. Comparative analysis of accuracy of SLA and DMLS technologies for cast partial denture frameworks using metrology software [Internet]. IP Ann Prosthodont Restor Dent. 2025 [cited 2025 Oct 20];11(1):46-53. Available from: https://doi.org/10.18231/j.aprd.2025.010
APA
Swami, R. S., Doddamani, M. H. (2025). Comparative analysis of accuracy of SLA and DMLS technologies for cast partial denture frameworks using metrology software. IP Ann Prosthodont Restor Dent, 11(1), 46-53. https://doi.org/10.18231/j.aprd.2025.010
MLA
Swami, Rajesh Suhas, Doddamani, Mallikarjun H. "Comparative analysis of accuracy of SLA and DMLS technologies for cast partial denture frameworks using metrology software." IP Ann Prosthodont Restor Dent, vol. 11, no. 1, 2025, pp. 46-53. https://doi.org/10.18231/j.aprd.2025.010
Chicago
Swami, R. S., Doddamani, M. H.. "Comparative analysis of accuracy of SLA and DMLS technologies for cast partial denture frameworks using metrology software." IP Ann Prosthodont Restor Dent 11, no. 1 (2025): 46-53. https://doi.org/10.18231/j.aprd.2025.010
