- Visibility 55 Views
- Downloads 12 Downloads
- DOI 10.18231/j.aprd.2025.018
-
CrossMark
- Citation
Smile with confidence: How implant-supported dentures enhance the quality of life
Introduction
In overdenture therapy, a complete removable denture is placed over dental implants, tooth roots, or remaining teeth. For over a century, practitioners have effectively aided the full denture treatment with pre-existing tooth structures or retained roots.[1] However, there are some disadvantages to the tooth-borne version of this treatment, such as issues with dental caries, periodontal disease, technical issues with making dentures, denture fracture, and the fact that working with a compromised, terminal dentition means that many practitioners are reluctant to recommend this treatment to their patients. It has been demonstrated that edentulous patients can be successfully treated with osseointegrated implants over the long term [2] Attachment-retained overdentures supported by implants are currently recognized as a viable therapeutic option. [3] Improving patient satisfaction and perfect mandibular denture retention are the two main goals of utilizing implants for these patients. [4], [5], [6], [7] When compared to fixed restorative procedures for edentulous individuals that require additional implants, this treatment is less expensive. A number of significant factors have led to the recent push toward endosseous dental implants as the support and retention mechanism for mandibular overdenture therapy.
In addition to offering many of the advantages of traditional toothborne overdentures, implant overdenture therapy eliminates some of the most problematic issues, like periodontal disease and tooth decay. [8] Even after all teeth have been extracted, dental implants offer a way to lay the groundwork for overdenture care. With implants, dentists can restore missing supporting components for patients who are edentulous and currently wear traditional complete dentures. Ultimately, the results of implant overdenture treatment are consistently and notably superior to those of traditional complete denture treatment. [9], [10] Implant-retained overdentures fit the mandible nicely, especially if the implants were positioned in the intercanine spaces. There are other attachment methods employed, but ball attachments have shown to be dependable. [11], [12] A spherical patrix that is screwed into the implant assembly makes up the ball attachment. Using either a replaceable elastic ring or spring-action arms, the matrix fits over the patrix and provides retention. There are two ways to connect the denture and matrix: directly and indirectly.
This article describes a clinical procedure for a direct connection between a complete mandibular overdenture and two supra implant nonsplinted ball attachments. This method prevents compression of the gingival peri-implant soft tissue, and allows the denture to be seated completely on the supporting surface.
Case Report
A loose lower full denture prosthesis was the main complaint of a 65-year-old female patient who presented to the Department of Periodontology, Faculty of Dental Sciences, SGT University. The patient's bottom denture was loose, making it difficult for the patient to speak or eat. The patient disclosed that she had experienced periodontal disease-related tooth loss fifteen years prior. She had a complaint of a loose mandibular complete denture for the last two months while wearing her existing set of dentures. Upon clinical examination, the patient's upper and lower arches are entirely edentulous. The mandibular ridge was discovered to have resorbed, although the ridge was U-shaped, smooth, and free of any irregularities, bone spicules, or fragments of root. The maxillary arch was advantageous for a denture rehabilitation.
To select implants, a panoramic radiograph was acquired and maxillary and mandibular diagnostic casts were created. Upon radiographic evaluation, the patient's mandibular anterior region exhibited dense, compact bone devoid of any disease. To rule out any pathology, the patient's blood reports were also examined. She was advised of her options for treatment, which included the use of implant therapy to create a removable prosthesis supported by two or four implants. The patient chose to have an overdenture placed over two single-piece dental implants with ball attachments placed on the mandibular arch.
Clinical procedure
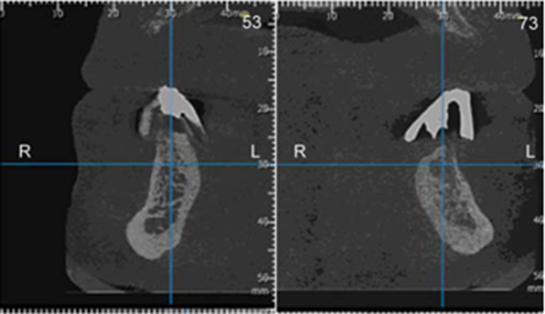
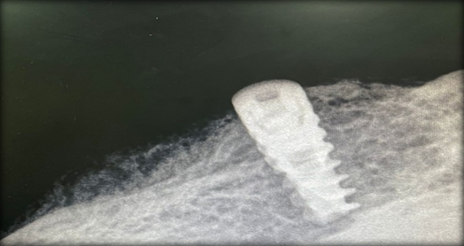
The patient's current denture was just made, and it was determined to be adequate in terms of occlusion, stability, and appearance. For this reason, an implant-supported overdenture prosthesis was created using the same prosthesis. To create the radiographic stent, a older mandibular denture was used as a stent. At the suggested implantation site, gutta-percha markers were inserted into the stent. The locations for implant placement, as well as the height and width of the bone, were determined using Planmeca 3D scans ([Figure 1]).
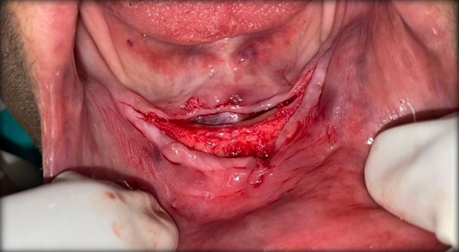
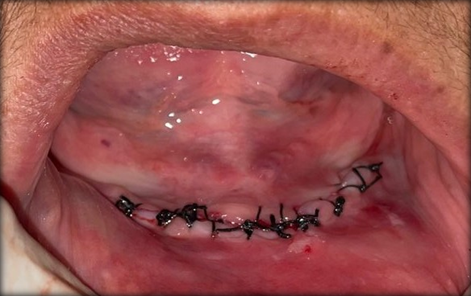
The patient's mouth's implant locations were marked using a surgical stent for a lower full denture prosthesis. Two 3.8 × 10 mm implants were inserted using an open technique between the mandible's mental foramen, with the implant site prepared via sequential drilling while adhering to sterile surgical protocol. For the mandibular denture to passively sit over the top of the implant ball attachment, the area where the implants were positioned had to be alleviated. To enable the patient to wear the prosthesis right once following surgery, a soft reliner (Coe-Soft Reliner, Dentsply) was placed within the denture in the implant location. Analgesics, ibuprofen (600–800 mg every 6–8 hours) and 0.12% chlorhexidine gluconate (twice daily for two weeks) were prescribed. After 24 hours, instructions were given to apply cold compression with an ice pack at 20-minute intervals ([Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10], [Figure 11]).

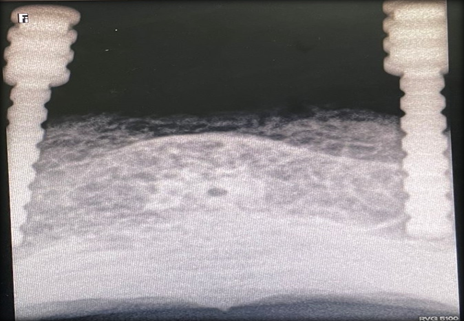
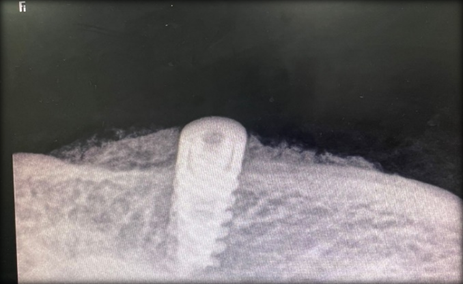




The liner that was positioned on the denture's tissue surface was taken out three months after the implants were inserted. The prosthesis of the patient was thoroughly inspected to guarantee passive fit. By using a rubber disk or separator, the neck of the O-ring attachment (the undercut area) was blocked. Using autopolymerizing resin, the keeper caps or restraint parts for the implant abutment were inserted straight into the denture's fitting surface (Dentsply Repair Material). After that, a typical chairside autopolymerizing resin mixture was made and inserted into the denture.After the denture was installed and the keeper caps were connected, the patient was instructed to close in function over the implants. The patient's denture was taken out of the mouth just before the final set, any extra acrylic material was taken out, and then the denture was put back in. Following the denture's finishing and polishing, intraoral occlusal equilibration was performed.
Discussion
In this article, an implant-supported overdenture prosthesis was created at a relatively modest cost, maintaining both function and aesthetics. The original complete denture prosthesis was retained. The cost of therapy would rise if an implant-supported fixed prosthesis required the implantation of more implants. Additionally, this process allows the prosthesis to be made from easily obtained and recognizable materials. In a study by Li Chen, patients restored with tooth-supported and implant-supported overdentures had superior comparative masticatory efficiency than patients restored with traditional complete dentures in the comparative masticatory efficiency test. After comparing the clinical results of several overdenture anchorage techniques, Naert discovered that all groups had 100% implant success after five years.He saw a 98% success rate after 52 months of observation. [13]
The overdenture prosthesis supported by implants aids in alveolar bone maintenance. According to Crum and Rooney, patients with complete upper and lower dentures had a 5.2 mm reduction in mandibular anterior height, whereas patients with overdentures had a 0.6 mm reduction. [13] Under an implant overdenture, the anterior mandibular bone may resorb as low as 0.5 mm over the course of five years, and long-term resorption may continue at 0.1 mm per year.The fixed implant full denture is no different. For a mandibular complete denture supported by a conventional implant, LoCascio and Salinas recommended a space of 15 mm from the mandibular ridge to the opposing dentition.In contrast, William recommended a space of 17 mm for an overdenture supported by framework, which is an extra 2 mm (for the fixed frame). There was 15 mm of available interarch space in the scenario discussed in this article. [14]
There are two ways to connect the retentive ingredient to the denture: directly and indirectly. To complete the relining procedure and link the matrix in the laboratory, the indirect technique involves placing the implants about the denture and recording the soft tissue support of the denture. The utilization of a single denture foundation acrylic resin and a shorter chair time are potential benefits of this technique. Nonetheless, there is a chance of inaccuracy when transmitting and registering the implant's position using analogs. Furthermore, the patient is not using the prosthesis at this moment. The direct method of intraoral ball attachment location is easy, quick, affordable, and preserves the patient's prosthesis. If relining the prosthesis is necessary, it ought to be finished first. Bulent presented a method of providing the precise relationship between the implant's component parts and the supporting tissues without applying pressure to the fingers. [15] It is important to note that this process is technique-sensitive, and the physician must ensure that the attachments are precisely placed on the implant abutments throughout the imprint process. A two-stage impression approach that accurately records implant components and the alveolar mucosa in a functional state was disclosed by Bulent and Volkan. [16] Compared to direct approaches, this technique has the drawback of being time-consuming. As long as the implants are precisely positioned parallel to one another, the direct procedure covered in this article is less time- and technique-consuming. Kenney and Richards' photoelastic research revealed that the ball/O-ring attachment reduced the amount of stress applied to the implants. [17] The overdenture is able to revolve around the ball that is attached to the implant body because it appears that the O-ring provides retention against forces that could dislodge it toward the occlusal surface. As a result of rotation, there was little stress on the implants and maximum wide stress distribution on the ridge in the posterior edentulous area. Therefore, it appears that the mandibular overdenture supported by implants in the interforaminal area preserves bone in the anterior jaw and enhances retention, stability, and chewing capacity. Solitary ball attachments seem to be less expensive, less method sensitive, and more accommodating for tapering arches when two implants were used in the front jaw to retain an overdenture. [18]
Conclusion
The edentulous subject's oral health-related quality of life is enhanced by the mandibular overdentures held in place by two ball attachments supported by two endosseous implants. This retains the less retentive mandibular denture prosthesis resulting from a poor mandibular foundation. It illustrates a scenario of an edentulous patient seeking an inexpensive way to increase denture retention. Comparing mandibular overdentures to traditional mandibular prostheses, notably fewer visits were needed for postplacement pressure spot adjustments. [19], [20]
Source of Funding
None.
Conflict of Interest
None.
References
- AH Fenton. The decade of overdentures: 1970-1980. J Prosthet Dent 1998. [Google Scholar]
- R Mericske-Stern, T Steinlin Schaffner, P Marti, AH Geering. Peri-implant mucosal aspects of ITI implants supporting overdentures. A five-year longitudinal study. Clin Oral Implants Res 1994. [Google Scholar]
- JS Feine, P De Grandmont, P Boudrias, N Brien, C Lamarche, R Tache. Within-subject comparisons of implantsupported mandibular prostheses: Choice of prosthesis. J Dent Res 1994. [Google Scholar]
- S Blomberg, PI Brånemark, GA Zarb, T Albrektsson. Tissue integrated prostheses. Psychological response 1985. [Google Scholar]
- J Hoogstraten, LM Lamers. Patient satisfaction after insertion of an osseointegrated implant bridge. J Oral Rehabil 1987. [Google Scholar]
- DR Burns, JW Unger, RK Elswick, JA Giglio. Prospective clinical evaluation of mandibular implant overdentures: Part IIPatient satisfaction and preference. J Prosthet Dent 1995. [Google Scholar]
- JS Feine, GE Carlsson, MA Awad, A Chehade, WJ Duncan, S Gizani. The McGill consensus statement on overdentures. Int J Oral Maxillofac Implants 2002. [Google Scholar]
- O Donatsky, S Hillerup. Non-submerged osseointegrated dental implants with ball attachments supporting overdentures in patients with mandibular alveolar ridge atrophy. A short-term follow-up. Clin Oral Implants Res 1996. [Google Scholar]
- AG Payne, YF Solomons. The prosthodontic maintenance requirements of mandibular mucosa- and implant-supported overdentures: a review of the literature. Int J Prosthodont 2000. [Google Scholar]
- D Van Steenberghe, M Quirynen, L Callberson, M Demanet. A prospective evaluation of the fate of 697 consecutive intraoral fixtures ad modum Branemark in the rehabilitation of edentulism. J Head Neck Pathol 1987. [Google Scholar]
- I Naert, S Gizani, M Vuylsteke, D Van Steenberghe. A 5-year randomized clinical trial on the influence of splinted and unsplinted oral implants in mandibular overdenture therapy. Part I: Peri-implant outcome. Clin Oral Implants Res 1998. [Google Scholar]
- L Chen, Q Xie, H Feng, Y Lin, J Li. The masticatory efficiency of mandibular implant supported overdentures as compared with tooth supported over-dentures and complete dentures. J Oral Implantol 2002. [Google Scholar]
- RJ Crum, GE Rooney-Jr. Alveolar bone loss in overdenture: A 5-year study. J Prosthet Dent 1978. [Google Scholar]
- M Quirynen, I Naert, D Van Steenberghe, C Dekeyser, A Callens. Periodontal aspects of osseointegrated fixtures supporting a partial bridge. An up to 6-years retrospective study. J Clin Periodontol 1992. [Google Scholar]
- T Jemt, J Chai, J Harnett, MR Heath, JE Hutton, RB Johns. A 5-year prospective multicenter follow-up report on overdentures supported by osseointegrated implants. Int J Oral Maxillofac Implants 1996. [Google Scholar]
- SJ Locascio, TJ Salinas. Rehabilitation of an edentulous mandible with an implant supported prosthesis. Pract Periodontics Aesthet Dent 1997. [Google Scholar]
- WG Golden, AG Wee, TL Danos, AC Cheng. Fabrication of a two piece superstructure for a fixed detachable implant supported mandibular complete denture. J Prosthet Dent 2000. [Google Scholar]
- B Uludag, K Cogalan, S Polat. An alternative impression technique for implant-retained overdentures with locator attachments. J Oral Implantol 2010. [Google Scholar]
- B Uludag, V Sahin. A functional impression technique for implant supported overdenture: A clinical report. J Oral Implantol 2006. [Google Scholar]
- R Kenney, MW Richards. Photoelastic stress patterns produced by implant-retained overdentures. J Prosthet Dent 1998. [Google Scholar]
How to Cite This Article
Vancouver
Chaturvedi A, Bhardwaj A. Smile with confidence: How implant-supported dentures enhance the quality of life [Internet]. IP Ann Prosthodont Restor Dent. 2025 [cited 2025 Sep 09];11(1):91-95. Available from: https://doi.org/10.18231/j.aprd.2025.018
APA
Chaturvedi, A., Bhardwaj, A. (2025). Smile with confidence: How implant-supported dentures enhance the quality of life. IP Ann Prosthodont Restor Dent, 11(1), 91-95. https://doi.org/10.18231/j.aprd.2025.018
MLA
Chaturvedi, Aditi, Bhardwaj, Amit. "Smile with confidence: How implant-supported dentures enhance the quality of life." IP Ann Prosthodont Restor Dent, vol. 11, no. 1, 2025, pp. 91-95. https://doi.org/10.18231/j.aprd.2025.018
Chicago
Chaturvedi, A., Bhardwaj, A.. "Smile with confidence: How implant-supported dentures enhance the quality of life." IP Ann Prosthodont Restor Dent 11, no. 1 (2025): 91-95. https://doi.org/10.18231/j.aprd.2025.018
