Introduction
In the past, implants were placed using the 'Bone-Driven Implant Placement' concept, prioritizing bone availability over ideal restoration position. This often resulted in compromised aesthetics and function. Advances in bone grafting materials, Guided Bone Regeneration (GBR) techniques, and implant surface technology have shifted the paradigm to 'Restoration-Driven Implant Placement.1
In 1989, Croll emphasized the importance of restoration design in achieving optimal dental aesthetics and function. He identified two crucial objectives which includes accurate replacement of missing tooth structure and reproduction of emergence profile.2
Implant therapy has become a vital aspect of surgical dental practice, with achieving optimal aesthetic outcomes being a primary objective. Meeting patient expectations is crucial to success, and soft tissue health and esthetics are key factors influencing patient satisfaction. However, achieving harmonious soft tissue integration remains one of the most daunting challenges for clinicians in implant restoration.3
A well-designed emergence profile is crucial for seamless integration of dental implant restorations with surrounding hard and soft tissues. In the aesthetic zone, the emergence profile of implant restorations must mirror natural tooth contours for optimal results. The emergence profile, first described by Stein and Kuwata in 1977, encompasses the critical transitions from soft tissue to tooth/crown contours. Achieving a natural emergence profile is essential for dental implant restorations, particularly in visually sensitive areas.4
Wohrle PS introduced the Nobel Perfect Esthetic Scalloped Implant, a design enhancing anterior aesthetic outcomes. Its scalloped profile preserves facial bone and soft tissue, optimizing emergence profiles.5
Attaining an ideal emergence profile requires careful consideration of multiple factors throughout the treatment process. When a suitable tissue foundation is present, the key to achieving optimal emergence profile lies in the thoughtful selection of Implant design and placement, healing abutment configuration and intermediate prosthetic components.6
Aesthetic implant-supported restorations require a natural transition between the restoration and soft tissues. Achieving an ideal emergence profile (EP) often necessitates customization. Factors influencing EP shape include Implant 3D position, Soft tissue quantity and provisional restoration contour. A well-designed provisional restoration is crucial for achieving an esthetic outcome.7
The aim of the present clinical report is to create emergence profile by using customized prefabricated abutment and transferring the soft tissue contour from provisional to the final restoration and fabrication of final implant restoration with predictable esthetic results.
Case Presentation
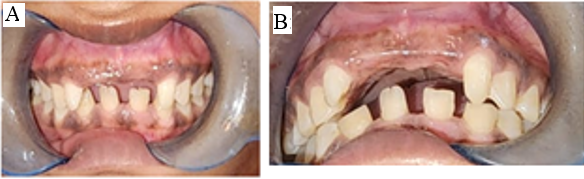
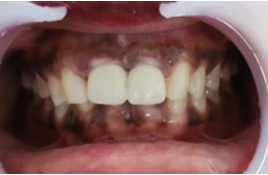
A 20 years-old female patient presented to the Department of Prosthodontics with missing right and left central incisors due to a traumatic accident years ago, had been restored with an acrylic removable partial denture. She wanted to replace her removable denture with a fixed solution. The clinical examination, radiographs, diagnostic casts, and photographs revealed an increased mesio-distal width of the edentulous space, a high lip-line and class II jaw relation with an overjet of 10mm and peg laterals.(Figure 1A,B)
Treatment planning
Patient was moderately healthy with no relevant medical history. Patient was explained about different treatment option. Dental implants and fixed partial dentures were clearly discussed, along with the pros and cons of each. She chose implant solution as she didn’t want to sacrifice any sound tooth structure of the adjacent teeth.
A preliminary impression was made to make a diagnostic cast. A diagnostic aesthetic wax-up was created to determine the treatment outcome. The patient had thick gingival biotype which was suitable for creating emergence profile around dental implant. Cone beam computed tomography was obtained to select the implant sizes. After thorough CBCT examination, implant sizes of two 3.3x11.5mm DIO implants were planned. Mesio-distal space necessitated composite buildup on mesial surfaces of both lateral incisors. An informed consent was obtained from the patient before starting the procedure.
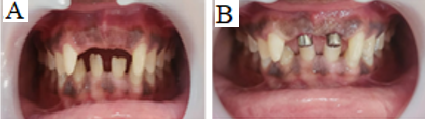
Routine blood investigations were performed and all the parameters fell under normal limits. Local anesthetic solution was administered using lignocaine 2% (1:80,000) and full thickness mucoperiosteal flap was reflected. Osteotomy was prepared using physiodispenser with sequential drilling and parallel pin angulations were checked to ensure final implant positioning.(Figure 2A) 3.3 X 11.5 mm diameter (DIO Dental Implant System) were placed.(Figure 2B) Then stability of implant was checked using torque rachet. Flaps were closed and sutured using Vicryl 4-0 non resorbable interrupted sutures.(Figure 2C) Post operatively patient was asked to take antibiotic amoxicillin & clavulanic acid 625mg thrice daily for 5 days. Analgesic Diclofenac sodium twice daily for 5 days. Patients was also asked to perform routine oral hygiene and advised to rinse with chlorhexidine gluconate for a period of 15 days. Patient was recalled after 2 weeks of surgery and sutures were removed and patient was advised to maintain the oral hygiene.
Figure 2
A: Parallel pin placed; B: 3.3×11.5mm DIO implants placed; C: Simple interrupted sutures were given
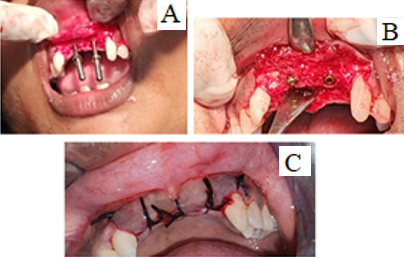
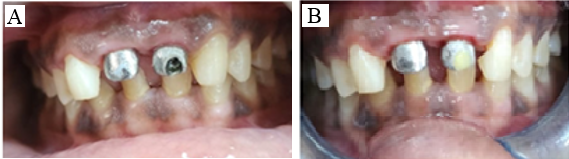
Removable prosthesis was given during healing period. After 3 months of satisfactory healing, stage II surgery was performed.(Figure 3A) The implant was in submerged position, so incisions were made in the implant site and flaps elevated conservatively to expose the cover screws .Cover screws were removed and replaced with healing abutment for one week. (Figure 3B)
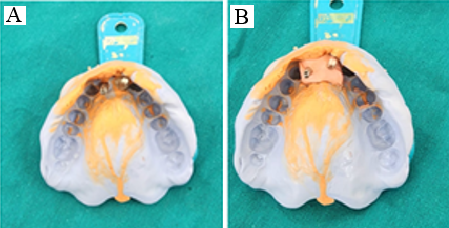
After one week healing abutments were removed and closed tray impression coping was screwed and impression were made with poly vinyl siloxane (AVUE GUM PUTTY).(Figure 4A) The impression coping was tightened to the lab analog and positioned back into impression,gingival mask (ESTHETIC MASK) was applied and cast was poured with TYPE III die stone.(Figure 9)
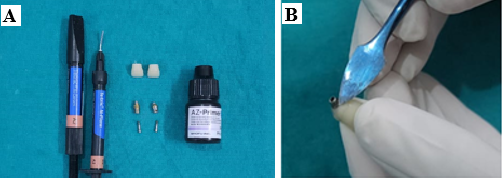
Acrylic tooth, metal primer (SHOFU AZ PRIMER), flowable and microfilled composite (Tetric N flow and ceram A2) were used for fabrication of provisional crowns (Figure 5A).
Prefabricated abutments were surface-treated with metal primer to improve the adherence of composite to the implant abutments and to create emergence profile of the provisional restoration (Figure 5B).
Figure 5
A: Acrylic tooth, metal primer, flowable and packable microfilled composite; B: Addition of composite to create emergence profile
Laboratory processed, screw retained provisional restoration were made.(Figure 6) The provisional crowns were contoured and highly polished to harmonize with the surrounding peri-implant soft tissue.
Figure 7
A: Screw retained provisional on 11 and 21; B: Provisional modified on subsequent visits. Composite build up done on lateral incisors

The patient preferred a gap-free smile, even with a slightly larger crown. Composite buildup has been done on both the lateral incisors and composite material was added to modify the provisional restoration.(Figure 7A) This method employs pressure in each stage to direct tissue growth. This dynamic compression technique in the aesthetic zone is a clinical method based on the initial pressure and subsequent modification of provisional restoration by adding composite material to mimic the natural tooth contour.
The patient was scheduled for multiple visits to monitor the gingival contouring progress. Composite resin was added wherever needed and polished, and the provisional crown was screwed and tightened.(Figure 7B) Once the gingival level was considered satisfactory for both the clinician and the patient, final impression was planned.
Final restoration
A provisional restoration was utilized as an impression coping to capture the final impression, replicating the emergence profile through to the definitive restoration.
The process involved:
Aesthetics were compromised due to the visible screw access hole on the labial surface of the central incisor. To overcome this limitation, a cement-retained and splinted restoration was designed to provide a more aesthetically pleasing solution.
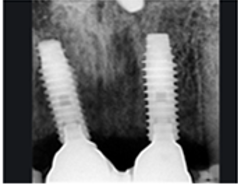
Customized screw retained metal abutments were fabricated and securely screwed into the implant.(Figure 9A) The access hole was sealed with Teflon and restored with flowable composite.(Figure 9B) Periapical radiographs has been taken to ensure the implant abutment connection.(Figure 10) Subsequently, a conventional impression was made using polyvinyl siloxane, and a master cast was poured".(Figure 11)
Figure 9
A: Customized screw retained metal abutments on 11 and 21; B: Access hole was sealed with Teflon and restored with flowablecomposite
A porcelain-fused-to-metal (PFM) restoration was planned as it combines strength and aesthetics. A wax pattern was fabricated on the cast for a splinted restoration. Splinted restorations provide additional stability since both were narrow diameter implants.
Following metal try-in, the splinted PFM fixed prosthesis was cemented with Glass inomer cement.(Figure 12, Figure 13) The patient was scheduled for a follow-up appointment three months post-cementation to assess the restoration's durability and overall satisfaction.(Figure 14, Figure 15) A subsequent evaluation revealed highly satisfactory outcomes with excellent soft tissue contouring around the implants and well-adapted peri-implant soft tissue, exhibiting optimal health and stability.
Discussion
The advancement of surgical implant therapy has enhanced osseointegration. However, prosthetic management of soft tissue in the aesthetic zone remains challenging, even after successful surgery. Literatures on Conventional loading implant techniques for soft tissue shaping with provisional restorations are limited.
This article presents a modified provisionals utilizing dynamic compression to model peri-implant soft tissue. The method employs pressure in the initial stage to direct tissue growth. An emergence profile is achieved with a prefabricated provisional restoration, and pressure is incrementally increased to avoid necrosis, anemia, or pain.
Limitations
Requires longer treatment duration.
Soft tissue tends to collapse after a short period if left unsupported.
Various techniques have been proposed to restore gingival contour, establish an emergence profile, and transfer the contour for an aesthetically pleasing final restoration.
Neale and Chee recommended recontouring tissues using gingivoplasty techniques before fabricating interim restoration which allows for precise shaping of gingiva to achieve desired emergence profile.7
Ormianer et al., immediately placed acrylic resin into the sulcus to transfer soft tissue shape but it has some potential drawbacks like chemical irritation of soft tissue from acrylic resin monomer and thermal irritation from polymerization process.8
Customized impression coping described by Hinds et al., which involves customizing impression coping to capture precise shape of gingiva.9
Recently advanced Digital impression techniques offers predictable digital reproduction of the emergence profile and peri-implant soft tissue contours. 10
Conclusions
Attaining exceptional anterior aesthetics requires patient selection, precise diagnosis, and thorough treatment planning, and staged treatment execution. From implant placement to post-operative care, careful consideration of critical parameters ensures a harmonious emergence profile. By combining functional and esthetic design principles, implant prostheses can meet high aesthetic standards. The dynamic compression technique provides a reliable conservative and effective alternative and minimally invasive solution for managing soft tissues in the aesthetically critical zone. By leveraging the elastic properties of gingiva and minimizing surgical interventions, this technique enhances aesthetic outcomes. Non-invasive gingival recontouring with temporary restorations enables incremental refinements, culminating in a seamless integration of soft tissue and restoration contours.