Introduction
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, also known as vaginal agenesis, is a congenital condition characterized by the underdevelopment or absence of the uterus and upper part of the vagina in individuals with a typical female karyotype (46, XX). Affecting approximately 1 in 4,500 female births, it is often diagnosed during adolescence when individuals do not menstruate, although they exhibit normal secondary sexual characteristics like breast development. Despite the absence of a uterus, the ovaries typically remain functional, allowing for normal hormonal production. The exact cause of MRKH syndrome is not fully understood but is believed to stem from a failure of th ce Müllerian ducts to develop during embryogenesis. While some genetic factors may be involved, most cases are sporadic. For those with MRKH, the absence of a fully formed vagina presents challenges in sexual function, particularly within the context of marital life.1, 2 Creating a functional vaginal canal becomes essential for sexual intercourse, and while fertility is impaired, sexual satisfaction can be achieved with proper intervention. Vaginal reconstruction can be achieved through two primary methods namely the non-surgical techniques, such as Frank’s method, which uses progressive vaginal dilators to expand existing vaginal tissue, and surgical techniques, including the McIndoe procedure, Vecchietti procedure, and laparoscopic neovaginoplasty. In both approaches, the use of prosthetic vaginal stents is essential to maintaining the canal's structure during the healing process, typically for several weeks to months, ensuring long-term success and functional outcomes.3 Prosthetic vaginal stents play a crucial role in maintaining vaginal patency following both surgical and non-surgical neovagina creation. These stents help maintain the structure of the newly formed vaginal canal and prevent scar tissue formation during healing. Various stent options, including custom-made or prefabricated silicone devices, are used based on individual anatomical needs.4
This case report highlights female patient with congenital MRKH syndrome, emphasizing the critical role of personalized prosthetic management in addressing vaginal agenesis. These case illustrate the significant impact such interventions have on improving sexual satisfaction and overall quality of life for individuals with MRKH syndrome.
Case Report
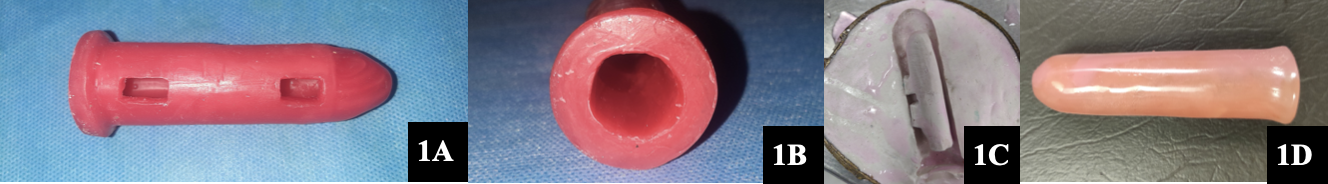
A 23-year-old female patient was referred to the Department of Prosthodontics by the Department of Gynecology for a customized vaginal stent prosthesis. Her medical history revealed a diagnosis of Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. The treatment plan involved creating a neovaginal cavity using the Abbe-McIndoe technique, for which a hollow vaginal stent was fabricated from heat-cure acrylic resin. Informed consent was obtained prior to treatment. Based on MRI scan data, the dimensions of the neovaginal cavity were calculated to be 7 cm in depth and 3 cm in width. A 5 ml syringe served as the base model for the stent over which 5mm of modelling wax (DPI, Modelling wax, Dental Products of India, Mumbai, Maharastra) layer added incrementally, which was modified according to the patient’s specific anatomical measurements. A smooth dome was shaped at the top end using modelling wax (DPI, Modelling wax, Dental Products of India, Mumbai, Maharastra), while the base of the syringe was left open in order to create hollow cylindrical configuration. Two windows were created on one side of the wax pattern shaft (Figure 1A). The pattern was invested in a conventional flask with dental plaster, then dewaxed to form a mould (Figure 1B). The mould was packed with heat-cure acrylic resin (DPI Heat Cure, Dental Products of India, Mumbai, Maharastra), and the stent was processed, trimmed, and cleaned. After disinfecting, the window openings and base of the hollow vaginal stent were sealed using self-cure acrylic resin (DPI Self Cure, Dental Products of India,Mumbai, Maharastra)(Figure 1C). The final stent was polished (Figure 1D) and inserted to maintain vaginal patency. Follow-up after six months confirmed that the desired patency had been successfully achieved.
Figure 1
Fabrication of hollow vaginal stent; A: Vaginal stent Wax pattern with two windows; B: Base of the Vaginal stent Wax pattern with Hollowness; C: Mold of the vaginal stent with a hollow cavity, created in a conventional flask following the dewaxing process; D: Final prosthetic Vaginal stent (The base and windows after processing sealed with Self cure acrylic resin).
Discussion
This case report, adhering to CARE guidelines, offers an in-depth evaluation of managing vaginal agenesis in Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome through the use of prosthetic vaginal stents. It highlights the pivotal role of prosthodontic intervention, particularly through a custom-designed heat-cure acrylic resin stent, integrated into the Abbe-McIndoe technique. The Abbe-McIndoe technique is a widely used surgical approach for creating a neovagina in individuals with vaginal agenesis. 3 The procedure involves creating a cavity between the rectum and bladder, which is then lined with a skin graft, typically harvested from the patient’s thigh or buttocks. For the graft to heal properly and maintain the shape of the neovagina, a prosthetic stent is critical. This stent acts as a scaffold, holding the cavity open, preventing the walls from collapsing or adhering, and ensuring the skin graft properly adheres to the vaginal lining.
The stent is customized based on the patient's anatomy, providing a personalized fit that enhances both comfort and functionality. The hollow design of the stent minimizes irritation and scarring, while allowing the graft to heal evenly, supporting long-term vaginal patency, which is vital for sexual function and overall quality of life. It is worn for several weeks to months post-surgery, playing a crucial role in the stability and structural integrity of the neovagina.
Despite its effectiveness, the use of prosthetic vaginal stents presents some challenges. Retention issues can arise, as the stent’s stability is highly dependent on the precise fit and the patient’s adherence to wearing it consistently. These factors can affect the stent’s ability to maintain patency and long-term success. Non-surgical methods, such as vaginal dilation or laparoscopic approaches, offer alternative treatments, but they may not achieve the same degree of anatomical reconstruction or functional outcomes as the Abbe-McIndoe technique. 4, 5, 6, 7, 8
The novelty of this case lies in the meticulous prosthetic involvement, showcasing the expanding role of prosthodontists in multidisciplinary care teams addressing complex conditions like MRKH syndrome. By incorporating advanced prosthetic designs, including custom-fabricated hollow stents tailored to patient-specific needs, the approach optimizes healing, reduces complications, and enhances overall quality of life. The significance extends beyond traditional prosthetic dentistry, demonstrating how innovative prosthodontic solutions contribute to successful management of vaginal agenesis. The case underscores the potential for advanced prosthetic interventions to become a standard in treating MRKH syndrome, offering both functional and psychological benefits for affected individuals.
Conclusion
This case report highlights the successful management of vaginal agenesis in Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome using a custom-fabricated hollow vaginal stent, demonstrating the pivotal role of prosthodontic expertise in complex multidisciplinary care.The challenges encountered with stent retention and patient compliance underscore the need for continued innovation in prosthetic design and patient management. By emphasizing the expanding role of prosthodontists beyond the oral cavity, this case illustrates how customized prosthetic interventions can significantly enhance patient quality of life. These findings support the potential for advanced prosthetic designs to become a standard in treating MRKH syndrome, improving both functional and psychological outcomes for affected individuals.

