Introduction
Artificial Intelligence (AI) has gathered significant attention in recent years due to its transformative potential across diverse industries, notably in healthcare.1 In the field of oncology, the integration of AI technologies represents a paradigm shift with profound implications for improving patient outcomes and advancing cancer care. 2 As AI continues to evolve, its application in oncology holds tremendous promises for enhancing the entire spectrum of cancer care delivery, from early detection and diagnosis to personalized treatment strategies and patient management. 3
The evolution of AI in healthcare is rooted in the pursuit of leveraging computational algorithms and machine learning techniques to analyse complex datasets and derive actionable insights. 4 From its inception, AI has aimed to simulate human intelligence and decision-making processes, enabling computers to perform tasks traditionally requiring human cognition. 5 In healthcare, AI's foundational principles encompass a diverse array of methodologies, including machine learning, natural language processing and deep learning, among others.
The rationale for integrating AI into oncology practice stems from the unique challenges and complexities inherent in cancer care. Oncology encompasses a broad spectrum of diseases characterized by heterogeneity, dynamic progression and varying treatment responses. Traditional approaches to cancer diagnosis and treatment often rely on subjective interpretation of clinical data and standardized treatment protocols, leading to variability in outcomes and sub-optimal patient care. AI offers a novel approach to address these challenges (Figure 2), by harnessing the power of data analytics, predictive modelling and decision support systems to optimize clinical decision-making and improve patient outcomes. 6
By analysing large volumes of clinical data, genomic information and imaging studies, AI algorithms can identify patterns, correlations and predictive markers that may elude human cognition. 7 This capability enables AI to facilitate early detection of cancerous lesions, predict treatment responses and tailor therapeutic interventions to individual patient characteristics.8 Moreover, AI-driven technologies hold the potential to streamline workflows, enhance diagnostic accuracy and empower healthcare providers with actionable insights to deliver personalized, evidence-based care. 9
Aims and Objectives
This article explores the impact of Artificial Intelligence (AI) in oncology, focusing on improving cancer detection, diagnosis, and treatment. It also addresses challenges in AI integration and future directions. The key objectives are:
Enhance Detection: Explore AI's role in early cancer detection.
Improve Diagnostics: Assess AI's impact on diagnostic accuracy.
Personalized Treatment: Investigate AI’s role in tailoring treatments.
Support Decisions: Examine AI-driven Clinical Decision Support Systems (CDSS).
Address Challenges: Identify issues like data privacy and bias.
Material and Methods
A comprehensive review of literature was conducted using PubMed, Google Scholar, and ScienceDirect databases. The search focused on studies published between 2019 and 2024. Search keywords included ‘Artificial Intelligence,’ ‘Cancer Diagnosis,’ ‘Precision Medicine,’ ‘AI Imaging in Oncology,’ and ‘Clinical Decision Support.’ Only peer-reviewed articles, reviews, and case studies that explored AI’s application in early cancer detection, diagnostic accuracy, and personalized treatments were selected. Data extraction focused on key advancements, including AI's role in precision oncology, imaging, and clinical decision-making. Ethical considerations, including data privacy and algorithmic bias, were also addressed.
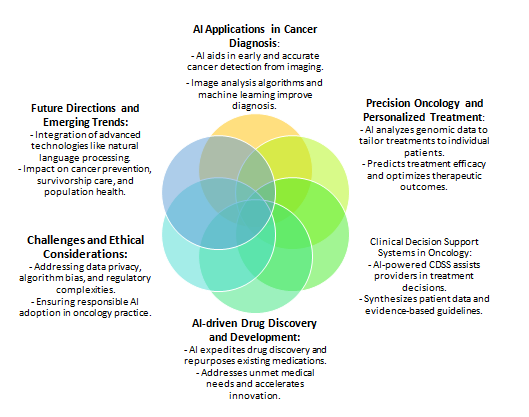
AI applications in cancer Diagnosis (Figure 1)
-
Importance of Early and Accurate Diagnosis
Improving Treatment Outcomes: Early detection of cancerous lesions plays a pivotal role in improving treatment outcomes and patient survival rates.
Timely Interventions: Enables healthcare providers to initiate appropriate interventions at an early stage when treatment options are more effective and less invasive.
Proactive Monitoring: Facilitates proactive monitoring and surveillance, allowing timely adjustments to treatment strategies based on disease progression and patient response.
-
Capabilities of AI-Powered Diagnostic Tools
Revolutionizing Diagnostic Imaging: AI has revolutionized diagnostic imaging by augmenting the capabilities of healthcare professionals and radiologists.
Image Analysis Algorithms: AI-powered tools utilize image analysis algorithms and machine learning models to analyze radiological images with high accuracy and efficiency.
Advanced Pattern Recognition: Leveraging pattern recognition techniques to identify subtle abnormalities and distinguish between benign and malignant lesions.
-
Advancements in AI-Driven Diagnostic Technologies
Real-Time Data Processing: State-of-the-art AI algorithms process vast quantities of imaging data in real-time, enabling rapid and accurate interpretation of radiological studies.
Deep Learning Architectures: Utilizing deep learning architectures and neural networks to extract meaningful features from medical images, facilitating the detection and characterization of cancerous lesions.
-
Impact on Cancer Detection and Diagnostic Accuracy
Improving Detection Rates: The integration of AI tools has led to significant improvements in cancer detection rates and diagnostic accuracy.
Reducing Diagnostic Errors: AI technologies help identify subtle signs of malignancy that may go unnoticed during manual interpretation, reducing diagnostic errors and false positives.
Enhancing Efficiency: Contributing to the efficiency of cancer diagnosis workflows and minimizing unnecessary follow-up procedures.
-
Predicting Chances of Recurrence in Breast Cancer
Software Utilization: Modern software leverages AI to predict the chances of recurrence in breast cancer by analyzing patient data, including genetic profiles, tumor characteristics and treatment history.
Personalized Risk Assessment: These AI-driven tools provide personalized risk assessments, helping clinicians develop more effective follow-up and treatment plans tailored to individual patients.
-
Precision Oncology and Personalized Treatment
Tailoring Therapeutic Interventions: Precision medicine focuses on individual patient characteristics, including genomic profiles, tumor biology and treatment response.
Role of AI: AI analyzes vast genomic datasets, identifies actionable mutations and predicts treatment efficacy, guiding personalized treatment strategies and optimizing therapeutic outcomes for cancer patients.
-
Clinical Decision Support Systems in Oncology
Assisting Healthcare Providers: Clinical decision support systems (CDSS) use AI algorithms to help healthcare providers make informed treatment decisions based on patient-specific data and evidence-based guidelines.
Enhancing Decision-Making: CDSS enhance clinical decision-making by synthesizing complex information, predicting treatment responses and recommending tailored therapeutic regimens.
AI-Driven Drug Discovery and Development
Expediting Drug Discovery: AI offers innovative solutions to expedite the drug discovery process by analyzing large-scale biomedical datasets and identifying potential drug targets.
Repurposing Medications: AI also assists in repurposing existing medications, addressing unmet medical needs in oncology and improving drug development success rates.
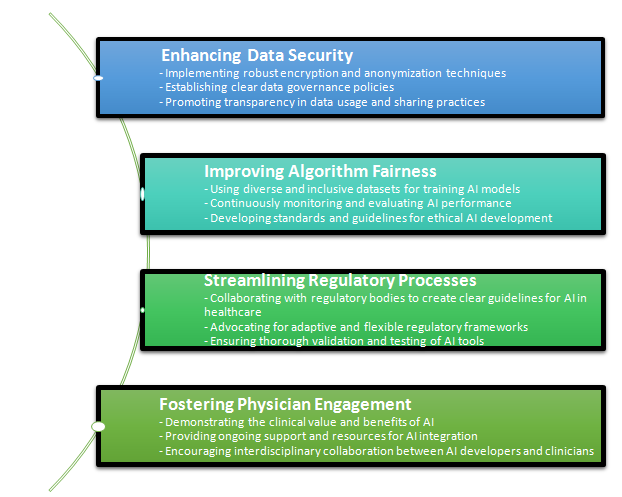
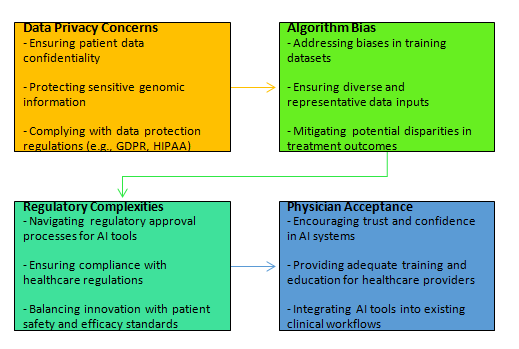
Challenges and Ethical Considerations
Data Privacy: Addressing data privacy concerns and protecting sensitive genomic information.
Algorithm Bias: Ensuring diverse and representative data inputs to mitigate biases in AI algorithms.
Regulatory Complexities: Navigating regulatory approval processes and ensuring compliance with healthcare regulations.
Physician Acceptance: Encouraging trust, providing adequate training and integrating AI tools into clinical workflows.
Future Directions and Emerging Trends
Ongoing Innovation: The future of AI in oncology involves continued innovation, collaboration and interdisciplinary research efforts.
Advanced Technologies: Integration of technologies such as natural language processing, robotics and augmented reality in cancer care.
Impact on Prevention and Survivorship: Potential impact of AI on cancer prevention, survivorship care and population health management.
Utilization of AI Technology in India
Healthcare Access: AI can help bridge gaps in healthcare access, particularly in rural and underserved areas.
Resource Optimization: AI tools can optimize the use of limited healthcare resources and improve diagnostic accuracy and treatment outcomes.
Collaborative Efforts: Encouraging collaboration between AI researchers, healthcare providers and government bodies to foster responsible AI adoption and innovation in oncology care.
Results
The integration of Artificial Intelligence (AI) in oncology has led to significant advancements across various domains of cancer care. AI-powered diagnostic tools have shown remarkable improvements in imaging, enhancing both cancer detection rates and diagnostic accuracy. By analyzing complex imaging datasets, AI algorithms can identify subtle abnormalities that might be overlooked by traditional methods. These improvements in diagnostic imaging have contributed to earlier detection of cancers, particularly in challenging cases where manual interpretation might lead to errors or delays.
In precision oncology, AI has revolutionized the personalization of cancer treatments by analyzing genomic and clinical data to tailor interventions. AI’s ability to identify actionable mutations and predict individual responses to therapies has made treatment plans more accurate, improving patient outcomes. This personalized approach, based on patient-specific data, allows for better-targeted therapies, minimizing side effects and increasing the likelihood of successful treatment.
Clinical Decision Support Systems (CDSS) empowered by AI have also played a crucial role in guiding oncologists through complex treatment options. These systems synthesize vast amounts of clinical information, offering evidence-based recommendations that support personalized care. As a result, oncologists are able to make more informed decisions, optimizing treatment strategies for each patient.
Despite these promising developments, challenges remain. Data privacy and the potential for algorithmic bias continue to raise concerns. AI models rely on large, diverse datasets, and any biases in the data can lead to disparities in care. Additionally, the regulatory landscape for AI technologies in healthcare remains complex, requiring clear guidelines to ensure that AI solutions are both safe and effective for widespread clinical use.
Discussion
The incorporation of Artificial Intelligence (AI) in oncology marks a significant shift in the approach to cancer care, offering substantial improvements across the cancer care continum. While AI's potential to revolutionize cancer care is evident, the practical implementation of AI-driven solutions presents several challenges and considerations that require careful examination.
AI-powered diagnostic tools have demonstrated the ability to improve the accuracy of cancer detection, particularly in radiological imaging and pathology. 10 These tools can analyze complex datasets, identifying patterns and abnormalities that may be missed by human observation. However, the reliance on large datasets for training AI models raises concerns about data quality, standardization, and representativeness. Variability in healthcare data across institutions and populations can affect the generalizability of AI algorithms, making it essential to ensure diverse and representative datasets in model training. 11
Furthermore, AI's role in precision oncology—tailoring treatments based on genomic profiles and individual patient characteristics—has opened new avenues for personalized medicine.12 Nevertheless, challenges persist in integrating AI-driven insights into clinical workflows, particularly in resource-limited settings where access to advanced technologies and genomic data is limited. Addressing these disparities is crucial to ensure equitable access to AI-enabled personalized care.
Clinical Decision Support and Physician Acceptance
Clinical decision support systems (CDSS) powered by AI have the potential to assist oncologists in making more informed treatment decisions by synthesizing complex data and providing evidence-based recommendations. 13 While these systems enhance decision-making, their adoption is contingent on physician trust and acceptance. Resistance to AI tools may stem from concerns about algorithm transparency, potential biases, and the perceived threat to clinical autonomy. 14 Therefore, fostering collaboration between AI developers and healthcare providers is vital to building trust and ensuring the seamless integration of AI into clinical practice.
Ethical and Regulatory Considerations
The deployment of AI in oncology also brings forth ethical and regulatory challenges as shown in (Figure 3). Ensuring patient data privacy and addressing algorithmic biases are paramount to safeguarding patient rights and maintaining public trust. 15 AI models trained on biased or incomplete datasets can perpetuate healthcare disparities, leading to suboptimal outcomes for under- represented groups. 16 Additionally, navigating the complex regulatory landscape for AI technologies in healthcare requires clear guidelines for algorithm validation, clinical testing, and approval. 17
Future Directions
Looking ahead, the future of AI in oncology is poised for continued innovation, with emerging technologies such as natural language processing, robotics, and augmented reality expected to further enhance cancer care.18 AI's potential impact on cancer prevention, survivorship care, and population health management holds promise for a more proactive and holistic approach to oncology. To maximize the benefits of AI, collaborative efforts between AI researchers, healthcare providers, and policymakers are essential. These collaborations will help address the ethical, logistical, and regulatory challenges associated with AI adoption in oncology, ultimately paving the way for a future where AI-driven cancer care becomes a standard of practice globally.
Conclusion
In conclusion, Artificial Intelligence holds tremendous potential for revolutionizing cancer care by enhancing diagnosis, treatment and patient management. As AI technologies continue to evolve, it is essential for oncologists, healthcare professionals and policymakers to embrace innovation, foster interdisciplinary collaboration and prioritize patient-centered care. By harnessing the transformative power of AI, we can advance the fight against cancer and improve outcomes for patients worldwide.