Introduction
Removable Prosthodontics offer a cost-effective treatment option for rehabilitation of partially edentulous patients resulting in an overall improved quality of life.1, 2 Distal extension cases pose a challenge in terms of stress distribution and retention of prosthesis. In such cases, extra-coronal semi-precision attachments, provide an esthetic alternative to conventional clasp design, minimize forces directed towards soft tissues and offer improved retention.3 However, the laboratory procedures involved in its fabrication are complex, time-consuming and require manual dexterity. The advent of digital technologies has revolutionized the procedure by effectively reducing the overall duration of prosthesis fabrication; eliminating chances of human errors, thus optimizing functional and esthetic outcomes.4 Presented here is this report, which is an integration of digital techniques with conventional protocols for rehabilitation of patient with an attachment retained cast partial prosthesis.
Case Report
A 36 year old female patient reported with a chief complaint of missing posterior teeth and difficulty in chewing since two years, for which she did not seek any dental treatment. Intra-oral examination revealed missing 36,37,46,47 (Figure 1). Alternate treatment options like fixed dental prosthesis and implant retained prosthesis were considered. Fixed dental prostheses were ruled out due to absence of a distal abutment. The patient was unwilling to undergo a surgical procedure for implant retained prosthesis and hence fixed- removable prosthesis was considered a suitable treatment option for rehabilitation of the patient. Treatment procedure was explained in detail and an informed consent was obtained.
Diagnostic mounting was done on a semi-adjustable articulator (Hanau Wide vue, Whip Mix) using a facebow transfer to evaluate the inter-occlusal space available which was found to be 6.5mm. which allowed the selection of Rhein 83 sagix attachment for the prosthesis.
Phase 1: Comprised of scaling and polishing, fabrication of porcelain fused to metal restorations over endodontically treated 14,16.
Phase 2/Prosthetic phase: Involved preparation of mandibular first and second premolars to receive the attachments. Gingival retraction was done, impressions made and cast was poured in dental stone. The digital protocol involved scanning of the cast using an optical scanner (Ceramill Map 400). The scanned data was saved in a.STL file and imported into the CAD software (Exocad Dental CAD; exocad GmbH).
Figure 3
A: Intra-oral trial of crown attachment resin assembly; B: Intra-oral trial of cast crown attachment assembly

Figure 5
A: Intra-oral trial of 3D printed resin framework; B: Trial of conventionally cast metal framework

Figure 6
A;B: Final impression; altered cast fabrication; C;D: Functionally generated path record; stone core fabrication

Figure 7
A: Teeth arrangement using Digital software; B: Checking Occlusion with opposing stone core; C: Defining denture base regions in digital software; D: Milling denture base and teeth as a single unit in wax disk; E: Additional milling of teeth using HIPC disk

Figure 8
A;B: Flasking wax assembly with metal framework and placing milled teeth in occlusal indentation in counterflask after dewaxing; C,D: Finished and characterised prosthesis

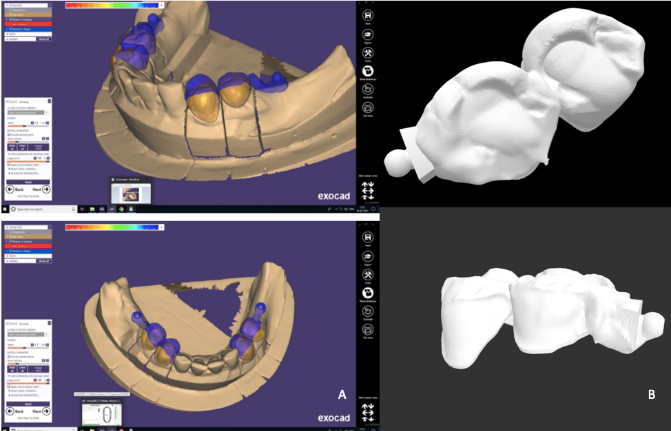
Designing the attachment
Designing involved selection of prepared margins and designing anatomic crowns over it. A cut back was prepared on facial surface of the crowns to give space for porcelain layering. Once the crowns were designed, the Rhein 83 sagix attachment was selected from the library of the software. The extension arm or the male component of attachment was inserted distal to last abutment keeping in view the relative parallelism, path of insertion and occlusal level of each attachment (Figure 2A). Once finalised, the. STL file (Figure 2B) was transferred into the printing unit (Rapid shape D30, Germany), where a 3 D printed resin (MAZICR D CAST) assembly was obtained. This resin assembly was tried intra-orally and checked for marginal fit, occlusal relationships, adaptation and (Figure 3A) was cast using conventional techniques. The porcelain layering on facial surface of copings was done. At this stage of bisque trial (Figure 3B), a pick up impression with the copings was made using a double stage putty wash impression technique with polyvinylsiloxane impression material (Zhermack Elite HD+).
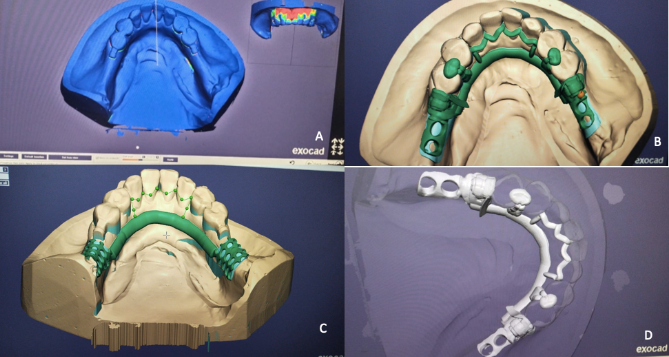
Digital designing of framework
The dental cast was scanned again. Digital surveying was done to assess the path of insertion. Digital blockout of undercuts was done. Designing involved the application of minor connectors, rests, finish lines and bar design. The female component or the matrix of attachment was designed using designing tool of the software (Figure 4A-D). The framework was printed in 3D castable resin material and tried intra-orally for fit and adaptation of the framework (Figure 5A). The framework was cast folowing conventional procedure. The splinted premolar crowns, with the Rhein 83 sagix attachment were luted in the patient's mouth. The cast framework containing the female housing, plus a silicone attachment was tried and fit was verified (Figure 5B).
Subsequently, the final impression was made and altered cast fabricated (Figure 6A, B)
Developing the functionally generated path
Dynamic occlusal relationship was recorded with functionally generated path with the cast metal framework in place. Occlusal rim made of pattern resin was created on the base plate and framework was placed intraorally. Patient was asked to close in centric occlusion to indent the soft pattern resin. The patient was instructed to protrude his/her mandible in forward direction without losing teeth-contact until the incisors were in edge-to-edge relationship. Similarly, the lateral excursive pathways were also recorded for both right and the left side till the material achieved complete set (Figure 6C). Modeling clay was used to block specified areas on the cast and then boxed. A stone core (Figure 6D) was obtained and mounted on a semi-adjustable articulator.
Record base and teeth arrangement
The articulated casts and mandibular cast with the framework in position were individually scanned. The .STL file obtained was transferred to the designing software where the teeth were arranged in confluence with the opposing stone core and were milled in HIPC (High impact polymer composite) block (Bredent). The artificial teeth and denture base assembly were milled as a single structure in a wax disc (Sigmadent)(Figure 7A-E).
Acrylization procedure
The conventional procedure for denture investment was followed. The wax milled artificial teeth and denture base assembly were invested in the cope of flask. After dewaxing, the artificial teeth and denture base assembly were removed from the cope of flask and the HIPC milled artificial teeth are placed in the indentation of teeth in an inverted manner. Following this, heat cure PMMA denture base material (Lucitone, Dentsply) was compression molded to complete the acrylization process (Figure 8A,B).
Insertion and Maintenance
The prosthesis was characterised by adding tissue coloured composite (Visio.Lign, Bredent,UK) to provide an uniqueness to the prosthesis. The prosthesis was then inserted (Figure 9). The patient was kept on regular follow visits to check the fit, function of the prosthesis and oral hygiene status.
Discussion
This case report describes a customised integrated conventional digital protocol where the framework casting, denture processing and record of dynamic occlusal relationship have been done using conventional protocol, whereas attachment incorporation, designing the components of framework, teeth arrangement and denture base design have used a digital protocol. The advantage of this digital-conventional method lies in the fact that due to the fabrication of a 3D printed resin model, lab procedures like cast block-out, duplication, wax pattern fabrication were avoided, thus saving the valuable laboratory and patient’s time.5, 6 Trial of the resin framework could be done, which was not possible with a conventional wax pattern; which helped in the evaluation of the framework. Also, the cost incurred in designing the 3D resin model was much lesser than the cost of milling of a metal framework, since the conventional casting procedure was carried out.7 Custom artificial teeth could be designed, which enabled a favourable interocclusal dynamic relationship.8 Since the conventional procedures of acrylization were followed, it allowed the formation of a strong bond between metal framework and resin base. 9
Incorporation of the attachments provided an increased retention of prosthesis and also increased the esthetic appeal due to absence of the conventional clasp arms. The fit and accuracy of the cast metal framework and the patient satisfaction with the prosthesis were excellent. 10
Clinical Ssignificance
Based on the results achieved in terms of improved functional and esthetic rehabilitation, it was observed, that this technique can be used as a successful treatment modality.