Introduction
Deformation of orofacial region may be congenital or acquired arising due to trauma or ablative cancer surgery. Intraoral defects often lead to asymmetry of the overlying soft tissue due to loss underlying supporting bone. Rehabilitation of patients with mandibular defects is a challenge to both surgeon and the rehabilitation specialist. The treatment goals are to restore form, function and esthetics. Recurrence of primary tumor or lesions arising as complication of post-adjunct therapy complicates the rehabilitation.
Major surgical procedures including segmental or marginal resection of mandible result in residual defects that require rehabilitation. Stents and guides serve as a template which allow resected bone and surrounding excised soft tissues to be guided back, thereby providing a platform for Prosthodontic rehabilitation.1
Rigid fixation has been used in the past for guiding the resected mandible. However due to complications such as fistula formation and introduction of newer techniques and materials, it is no longer in use.
The challenges in the case presented were the reduced mouth opening due to scarred tissue contracture and gross mandibular deviation. This paper describes a method where mandibular deviation in post mandibulectomy defect was managed with a combination approach using guide flange prosthesis and MMF screws with elastics.
Case Report
A 53 yrs old male patient was referred from division of Oral and maxillofacial surgery for rehabilitation of mandibulectomy defect. Past history revealed that the patient was diagnosed with oropharyngeal carcinoma 04 years back for which he received radiation therapy for 03 months. He was free from primary tumor or any metastatic foci and was asymptomatic until 06 months back, when he noticed a slow progressing swelling on Left(Lt) side of face, with mild, dull, aching pain.Biopsy of the lesion revealed osteoradionecrosis of mandible (Lt) and a segmental resection distal to mandibular first premolar was carried out. Patient reported to the department for rehabilitation after 02 weeks of surgery.
Extraoral examination revealed asymmetric face with mandibular deviation of 15mm towards left side and a reduced mouth opening of 08mm. Intraoral examination revealed poor oral hygiene, multiple cervical carious lesions, root stumps with missing teeth in the mandibular second premolar to molar region on Lt side (Figure 1). Patient was unable to bring teeth in maximum intercuspation. Based on history and clinical findings, a diagnosisof Class II(Cantor and Curtis) mandibular defect was arrived at.2 Treatment plan was formulated, discussed with the patient and an informed consent was obtained.
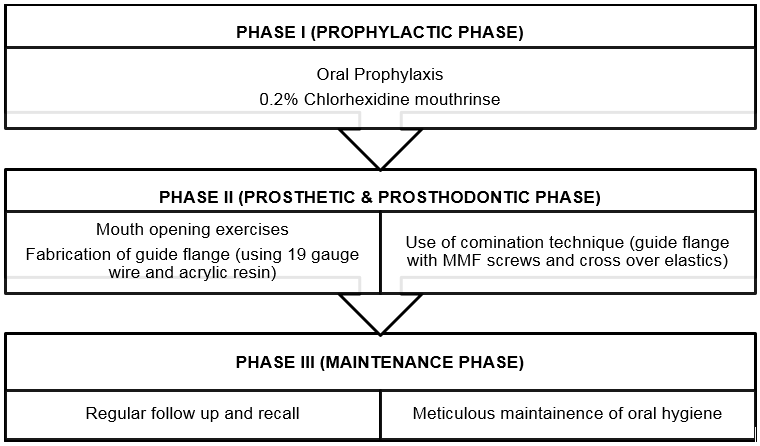
Treatment comprised of three phases. (Figure 5 )
Phase I: (Prophylactic phase)
Phase II: (Prosthetic and Prosthodontic phase)
Phase III: (Maintenance phase)
Phase I comprised of oral prophylaxis and 0.2% chlorhexidine mouthrinse prescription. Extractions of remaining root stumps and use of ultrasonic scaler could not be done due to risk of flare up of osteoradionecrosis.
Phase II comprised of fabrication of mandibular guide flange prosthesis to help guide the teeth into maximum intercuspation and ensure repeated closure at this position for adequate mastication.
Mouth opening was improved by using ice cream stick method.3 Diagnostic impressions were made using irreversible hydrocolloid (Algin-gum India), custom tray was fabricated and final impressions were made using two stage putty wash technique with polyvinyl siloxane elastomeric impression material (Affinis, Coltene, India). Inter occlusal records were made using bite registration wax(MAARC, India) by guiding the lower jaw into maximum intercuspation possible by external pressure. Casts were fabricated using type III dental stone (Kalstone, Kalabhai, India), and mounted on a mean value articulator.
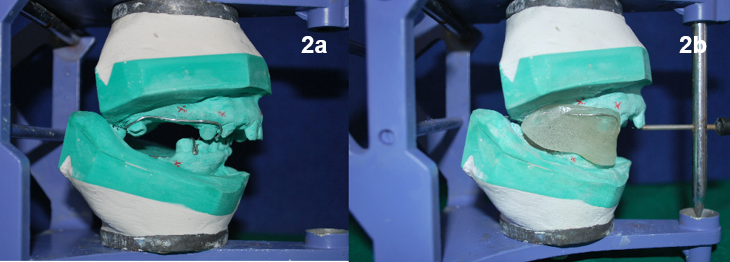
For fabrication of guide flange, 19 gauge/0.9mm SS wires were used for wire bending enveloping maxillary third molar buccally at level of attached gingiva upto maxillary premolars. Occlusal cross overs were made and the same wire was extended from lingual part of mandibular premolar to mandibular third molar (Figure 2). Acrylic shields were fabricated on buccal and lingual side to guide the mandible into planned intercuspation position using clear autopolymerizing acrylic resin (DPI Auto cure denture base material, India).Minor adjustments were made and the guide flange was inserted in the patient’s mouth. The patient was unable to hold the prosthesis in position as the scar tissue and muscle contracture on affected site exerted strong traction leading to destabilization of prosthesis.
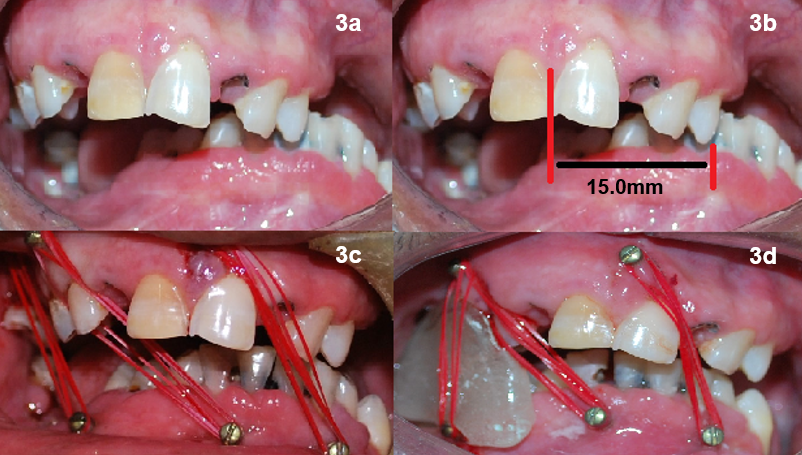
In consultation with the Oral & Maxillofacial surgeon, a combination method of using maxillomandibular fixation (MMF) screws and guide flange was planned (Figure 3). Three MMFscrews of 2 x 10mm were placed in maxilla in the region of central incisors, canines and premolars and 2 x 12mm screws were placed in mandible in the region of premolar of contralateral side, central incisor and canine of same side. These MMF screws were joined using cross-elastics. The screws were with minimum surgical intervention. They were left in position for 04 months with regular follow up for 1,3,7 days and every 02 weeks subsequently.
Phase III: Regular check up and maintenance of guide flange till occlusion improved for fabrication of a definitive prosthesis. Patient was recalled daily for the first week and thrice a week subsequently to ensure oral hygiene maintenance. The elastics which were broken or missing were replaced. This produced marked improvement in guiding the mandible to near maximum normal positionwith improved facial esthetics (Figure 4 ).
Figure 1
[a. Preoperativeextraoral showing deviation of mandible; b. Intraoral maxillary arch; c. Intraoral mandibular arch]

Discussion
Prosthetic Splints have been used to prevent rotation of fragments caused due to uneven muscle action in case of trauma. They allow healing of supporting tissues and help to achieve desired occlusal relationship. 1
Mandibulectomy is defined by Glossary of Prosthodontic terms(GPT-9) as the ‘surgical removal of a portion or all of the mandible and the related soft tissues and mandibular resection prosthesis is a maxillofacial prosthesis used to maintain a functional position for the jaws, improve speech and deglutition following trauma and/or surgery to the mandible and/or adjacent structures’.
According to Cantor and Curtis(1971),2 mandibular defects can be classified as
Class 1: Radical alveolectomy with preservation of mandibular continuity
Class 2: Lateral resection of mandible distal to cuspid
Class 3: Lateral resection of mandible extending upto midline
Class 4: Lateral bone graft surgical reconstruction
Class 5: Anterior bone graft surgical reconstruction
Class 6: Reconstruction of anterior portion of mandible without reconstructive surgery to unite lateral fragments.
Deviation of mandible towards defect site is often encountered in patients where continuity of mandible is lost due to tissue scarring and wound closure contracture. This counteracts the effects of elevator muscles causing deviation of mandible.3 Ideally, it is recommended that a guidance flange be fabricated presurgically and used immediately post-surgery to allow muscle balance and scarring to occur in a desirable manner.4, 5
The mandibular guidance prosthesis can be of two types:
(1) Palatal based guidance prosthesis including inclined plane prosthesis, widened maxillary occlusal table 6
(2) Mandibular based guidance prosthesis. It consists of RPD framework with a flange extending 7 to 10 mm laterally and superiorly on buccal aspect of premolars and molar on non defect site. The flange engages maxillary teeth during closure, thereby directing mandible to appropriate intercuspal position.
Cast metal guidance prostheses and attachments have been mentioned in literature for guidance of resected mandible. 7, 8 However, these appliances are complex, technique sensitive and expensive. Maxillomandibular fixation using only arch bar and elastics have been used in past but are rarely used now. Aramany and Myers,9 and Ackerman10 advocated use of intermaxillary fixation or guidance prosthesis immediately and showed the success of using these methods of rigid fixation. They treated 12 patients using maxillomandibular fixation in form of arch bars and elastics. In this case, we utilized a novel approach by using MMF screws as the number of teeth to retain an arch bar were less and the remaining teeth were carious and weak. The strength of this approach is that it can be used as an adjunct to conventional guide flange prosthesis in cases where muscular forces hamper the stability of the prosthesis especially in those cases reporting post-surgery. However rigid fixation demands increased maintenance of oral hygiene, regular follow up and should be used with care and under proper supervision in conditions like osteoradionecrosis. The loss of screws is also not uncommon with MMF screws. The acrylic guide flange prosthesis is simple and cost effective method for managing mandibular deviation.
Conclusion
Guide flange prosthesis may be used as a training device to allow closure in optimum occlusal relationship achieving maximum masticatory efficiency. Early prosthodontic intervention permits better occlusal contacts. With the time lapse, redirectiion of mandible to reduce deviation becomes complicated. Various supporting modalities facilitate closure of mandible by restricting unopposed muscle action. However, it is important to weigh the advantages and disadvantages before any technique is applied. Meticulous observation and care is imperative formaximum benefit to the patient forfavorable rehabilitation outcome.