Introduction
Mucormycosis is an aggressive fungal infection which commonly involves the nose and paranasal sinuses of the head and the neck region. This is caused by saprophytic aerobic fungi of the class Phycomycetes and hence this disease is also called as Phycomycosis.1 Immunocompromised patients are highly prone to develop this disease and its complications, where in the spores colonize in upper respiratory tract, germinate, develop hyphae and invade blood vessels and surrounding tissues.2 The devitalised tissue due to thrombosis and tissue necrosis results in continued fungal growth thus making it aggressive. 3 Once the fungal growth is established in paranasal sinus, the infection easily spreads and enters the orbit through nasolacrimal duct and may spread to brain through orbital vessels and cribriform plate. Patients with orbital involvement might have ophthalmoplegia, proptosis and intra nuclear sixth cranial nerve palsy. 4, 5 Due to aggressive and invasive nature of the disease, extensive surgical resection is required which results in large complex maxillofacial defects.
Even though surgical reconstruction is the preferred choice to manage these residual surgical defects, prosthetic rehabilitation is resorted to many a times because of the inherent advantages like, ease of covering large defects, multiple surgeries are avoided, predictable cosmetic results, ease of detection of the recurrence and is ideal for patients with advanced age and compromised health. 6 Maxillary resection without involvement of the orbit is relatively simpler to rehabilitate usually with hollow bulb obturator.
Extensive maxillary resection along with exenteration of the orbital contents leads to complex maxillofacial defect that needs rehabilitation with obturator along with orbital prosthesis. In such cases achieving optimum retention for the orbital prosthesis is a challenge and is usually retained by retentive attachment fixed to bulb of the obturator in the form of magnets or buttons. Due to absence of infraorbital bone, the obturator lacks vertical support and stability, and attached orbital prosthesis tends to move during mastication.
Case Report
A 60 year-old female patient reported to dept of otolaryngology with complaint of swelling over right maxillary region and diminished vision. She presented with a history of uncontrolled diabetes mellitus. Examination revealed an ulcerative lesion on hard palate, foul smelling rhinorrhoea, ptosis in right eye along with facial palsy on right side. Right Inferior turbinate tissue was taken for biopsy through endoscope. Histo-pathological examination revealed focal areas of necrosis with broad branching hyphae. MRI revealed enhancement in right masticatory space and parotid gland, non homogeneous densities in right maxillary and frontoethmoidal sinus along with mild oedema in perineural sheet of right optic nerve. NCCT of PNS and orbit revealed eversion of anterior and lateral walls of right maxillary sinus and right alveolar process of the maxilla. Based on clinical, radiological and histopathological findings, diagnosis of sinoorbital mucormycosis was arrived at.
Surgical treatment plan was formulated that comprised of total maxillectomy, exenteration of the orbit and total parotidectomy on right side. It was discussed with the patient, informed consent obtained and executed. Eight weeks after surgery, she was referred to department of Prosthodontics for rehabilitation.
Extraoral examination revealed a well healed residual orbital bed with fibrous band around the orbit post exenteration. Intraoral examination revealed well healed residual maxillary defect with communication between the orbital cavity and maxillary defect due to resected infraorbital floor and collapsed cheek on right side post maxillectomy. The contralateral arch had adequate periodontal support and stable occlusal contacts (Figure 1).
Treatment plan was formulated to rehabilitate the patient with a combination prosthesis comprising of an obturator and an orbital prosthesis. It was divided in four stages.
Stage I - Fabrication of palatal and bulb portion of the obturator.
Stage II- Establishment of occlusion.
Stage III- Customization of attachment between obturator bulb and orbital prosthesis .Stage IV- Fabrication of extraoral prosthesis.
In stage one, impression of the maxillary defect was made with irreversible hydrocolloid impression material, beading and boxing done and cast was fabricated. Hollow bulb obturator was fabricated with heat polymerized acrylic resin (Figure 2). This enabled the patient have food orally and Ryle’s tube was removed by the otolaryngologist.
In stage II, Occlusal rim was fabricated on the obturator, maxillomandibular relations recorded, articulation done, teeth setting carried out and prosthesis was acrylized, finished and polished (Figure 3).
The challenges in this case were to achieve retention for the orbital prosthesis that was obtained from bulb portion of the obturator and the passivity of retentive attachment between obturator and orbital prosthesis so that movement of the orbital prosthesis could be minimised during function.
To achieve this, custom attachment was fabricated using brass cylinder and housing. Housing was attached to the bulb of the obturator and cylinder was fixed to the orbital prosthesis. Retention to the extraoral prosthesis was provided by the brass cylinder when engaged in the housing. Since there was movement of brass cylinder within the housing, it acted like a movable joint and minimized the movement of the orbital prosthesis (Figure 4).
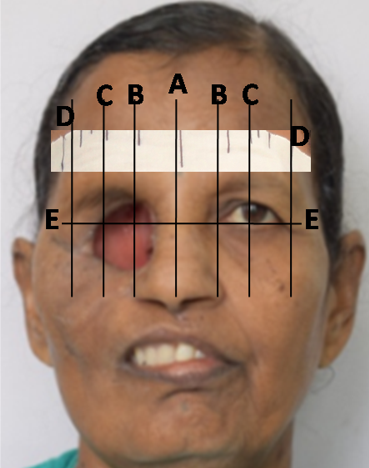
In Stage III, Impression of the orbital defect was made with irreversible hydrocolloid impression material, beaded, boxed and poured with dental stone to fabricate the moulage. Acrylic shell was fabricated on the orbital moulage which supported ocular prosthesis and brass ring of the customized attachment. Acrylic shell was tried in the orbital defect. Closely matching stock eye with that of the natural eye was selected. The patient was comfortably seated in a chair with natural head position (NHP) maintaining the left eye in a conversational gaze. Facial measurements were used to orient the shell according to gaze of the patient and series of vertical and horizontal lines were marked on a tape A) through the midline of the face (B) through the medial canthus, (C) through the pupil, (D) through the lateral canthus, pupil of the right eye. (E) through the inferior border of pupil; to achieve mediolateral and superoinferior position of the ocular shell as close to the unaffected eye as possible (Figure 5). It was attached to the acrylic shell with autoploymerizing acrylic resin. Wax pattern of the eyelids was carved on the acrylic shell and stock eye, tried on the patient to confirm the shell position, lid aperture and patient’s approval was obtained. Wax pattern was flasked, dewaxed and packed with HTV silicones (Figure 6).
Silicone portion of the prosthesis was attached to the acrylic shell and stock eye with the help of acrylic adhesive supplied with the system. False lashes were attached to the silicone lids to mimic natural appearance.
The prosthesis was delivered to the patient and post insertion instructions about maintenance, insertion and removal of the prosthesis were given to the patient
(Figure 7). Review protocol was formulated to recall her at the interval of 3 months for initial 1 year followed by every 6 months.
Discussion
During the rehabilitation of cases with mucormycosis the following guidelines need to be considered and followed.
Effective management of mucormycosis depends on early detection, diagnosis and extensive surgical resection of the involved tissues. 7
Prompt correction of comorbidities such as uncontrollable diabetes mellitus reduces mortality and morbidity
Maxillofacial rehabilitation is a multidisciplinary task and pre-surgical discussion with operating surgeon is essential to explore the possibility of creating favourable tissue undercuts to retain the prosthesis. 8
Prosthesis retention is achieved through teeth or tissue undercuts. Preventive and restorative dentistry needs to be emphasised upon to salvage as many teeth as possible
Incorporation of non-rigid retentive attachment between obturator bulb and the extraoral prosthesis helps reduce the movement during function.
Regular frequent follow-ups of the patient to rule out recurrence and to evaluate retention and stability of the prosthesis.
The challenges in this case were the extensive resection making it difficult to assess the optimum position of the iris and achieving adequate retention. Various methods for iris placement have been mentioned in the literature such as facial measurements using anatomic landmarks, ocular locator, inverted anatomic tracings, graph grid method, grid cutouts placed on spectacle frame, graph grid frame attached to spring bow, Modified Hanau wide view spring bow, cusyomised scale, optical vernier interpupillary distance ruler, Digital photograph. 9, 10, 11, 12, 13, 14, 15
Various methods of retention advocated in literature include spectacle frame, extensions from the obturator, magnets and buttons, engaging tissue undercuts, adhesives or osseointegrated implants. 16 In cases with multiple defects secondary to maxillectomy and orbital exenteration, obtaining retention between obturator bulb and orbital prosthesis with rigid connection such as magnets or buttons, results in movement of extraoral prosthesis when obturator is in function. 17 To reduce the movement of the prosthesis, custom-made retentive attachment with brass cylinder and housing was utilised.
Conclusion
This clinical report describes prosthetic rehabilitation of residual maxillary and orbital defects secondary to mucormycosis with an innovative method of achieving retention for orbital prosthesis from obturator bulb in a complex defect. The prosthesis thus fabricated was economical, biocompatible, esthetic, comfortable to use, easy to fabricate and clean and provided optimum functional and esthetic rehabilitation of the patient.