Introduction
Nanotechnology is the product of functional materials and structures in the Nano scale, using various physical and chemical methods.1 The particles of the length scale 1-100 nm are used. These are known as Nanoparticles. The US National Nanotechnology Initiative defines nanotechnology on three requirements, technology development at the atomic, molecular or macro level in the length scale of 1-100nm, creating and using structures, devices and system that have novel properties and functions because of their small or intermediate size and ability to control or manipulate on the atomic or molecular scale. 2 Over the past few decades, inorganic nanoparticles, whose structures exhibit significantly novel and improved physical, chemical, and biological properties, phenomena, and functionality due to their Nano scale size, have elicited much interest. Nano phasic and nanostructured materials are attracting a great deal of attention because of their potential for achieving specific processes and selectivity, especially in biological and pharmaceutical application. 3, 4 Recent studies have demonstrated that specifically formulated metal oxide nanoparticles have good antimicrobial activity or mechanical strength. 5 Among inorganic antimicrobial agents, silver has been employed most extensively since ancient times to fight infections and control spoilage. 6, 7, 8 The use of such nanoparticles has become very popular in the design and development of many dental materials so as to improve their chemical, physical and mechanical properties.
What is nanotechnology?
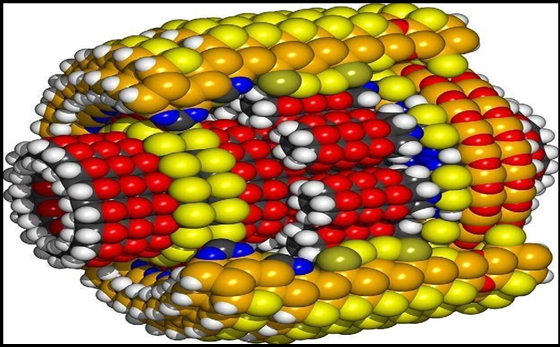
Nanotechnology is the engineering of functional systems at the molecular scale (Figure 1).
It is a highly multidisciplinary field and can be seen as an extension of existing sciences into the nanoscale, or as a recasting of existing sciences using a newer, more modern term.
Broadly, nanotechnologies consist of three mutually overlapping and progressively more powerful molecular technologies
Nanoscale-structured materials and devices that can be fabricated for advanced diagnostics and biosensors, targeted drug delivery, and smart drugs.
Molecular medicine via genomics, proteomics, artificial biorobotics (microbial robots). 7
Molecular machine systems and medical nanorobots allow instant pathogen diagnosis and extermination, and efficient augmentation and improvement of natural physiological function.
Approaches used in nanotechnology
Following approaches have been followed in production of nanoparticles, namely Bottom up approach, Top down approach and functional approach. The functional approach disregards the method of production of a nanoparticle, and the objective is to produce a nanoparticle with a specific functionality.
Bottom up technique
This technique seeks to arrange smaller components into a more complex assembly. The dental procedures employed are Local anesthesia, Hypersensitivity cure, Nanorobotic dentrifice (dentifrobots), Nano toothpaste, Dental durability and cosmetics, Orthodontic treatment, Photosensitizers and carriers, Diagnosis of oral cancer (nanodiagnosis), Whole tooth replacement, Tooth renaturalization, Nanodiagnosis, Treatment of oral cancer, Dental biomimetics, Endodontic regeneration, Nano terminators.9
Top down technique
In this technique smaller devices are created by using larger ones to direct their assembly. So, small features are made by starting with larger materials patterning and carving down to make nanoscale structures in precise patterns. Complex structures containing hundreds of millions of precisely positioned nanostructures can be fabricated. Materials are reduced to the nanoscale and can suddenly show very different properties, enabling unique applications.
As the size of system decreases there is increase in ratio of surface area to volume and number of physical phenomena becomes noticeably pronounced. This technique seeks to create smaller devices by using larger ones to direct their assembly. It includes Pit & fissure sealants, Bone targeting Nano carriers and other products. The dental procedures employed are Nanocomposites, Nano Light- Curing Glass Ionomer Restorative, Nano Impression Materials, Nano-Composite Denture Teeth, Nanosolutions, Nanoencapsulation, Plasma Laser application, Prosthetic Implants, Nano needles, Bone replacement materials, Nano-particulate based disinfection in endodontic.10
Functional approach: In this approach, components of a desired functionality are developed without regard to how they might be assembled. Other approaches followed at Rice University are given as follows.
Wet nanotechnology: Study of biological system that exist mainly in water environment, which include genetic material, membranes, enzymes, and nano- sized cellular components.
Dry nanotechnology: It derives from surface science and physical chemistry focuses on fabrication of structure in carbon, silicon and other organic materials.
Computational nanotechnology: It permits the modeling and stimulation of complex nanometer scale structure, the predictive and analytical power of computation is critical to success in nanotechnology.11
Applications of nanotechnology with examples
Types of nanotechnologies
Nanopharmaceuticals-Application include Cancer, Antiviral agents, Arteriosclerosis, Lung disease and diabetes, Gene therapy, Tissue engineering, Tissue cell repair
Nanodevices- Application include delivery of diagnostic and therapeutic agents They can be generally divided into three potent molecular technologies
Nanoscale materials and devices to be applied in advanced diagnostics and biosensors, targeted drug delivery and smart drugs.
Molecular medicine through genomics, proteomics, artificial biobotics (microbial robots)
Molecular machines and medical nanorobots aid in immediate microbial diagnosis and treatment and enhancement of physiological functions
Nanoparticles in Prosthodontics
Acrylic resin
The importance of acrylic resins in dentistry is evident. They are widely used in making temporary prosthetic base materials, provisional prosthesis, dentures and orthodontic removable appliances such as retainers and functional appliances. These resins commonly consist of methacrylates, especially poly methyl methacrylate (PMMA), and additional copolymers.12 However one of the major problems that patients and dentists commonly faced using these removable acrylic appliances is their potential for plaque accumulation due to surface porosities and food retentive configuration, which in turn increase bacterial activity of cariogenic oral flora.13
Titanium dioxide nanoparticles have been used as additives to biomaterials in order to induce antimicrobial properties.14, 15 Antimicrobial activities of titanium dioxide against candida albicans, staphylococcus aureus, pseudomonas aeruginosa, escherichia coli, lactobacillus acidophilus, etc. have been proved by recent studies.16, 17, 18, 19 Along with prominent catalytic effect, other characteristics such as white color, low toxicity, high stability and efficiency as well as availability20, 21 have made titanium dioxide an appropriate antimicrobial additive for use in acrylic resin.
Among compounds as inorganic carriers such as apatite, zeolite and phosphate, Silica dioxide is more promising due to its porous structure and adsorption properties. Nanoparticles of silica dioxide possess extremely high surface activity and adsorb various ions and molecules. 22 Silver nanoparticles due to their small size possess greater dispersion in PMMA matrix and produce larger area for oxidation. 23 The release of silver ions plays the major role in the antibacterial mechanism of silver nanoparticles by rupturing the cell wall causing protein denaturation, blocking cell respiration, and finally causing microbial death. 24
Tissue conditioner
Tissue conditioners have been commonly used to enhance the recovery of denture bearing tissues from trauma, damage or residual ridge resorption usually caused by ill-fitting dentures. Tissue conditioners could be kept clean by mechanical and chemical methods but this can cause considerable damage to tissue conditioners. 25, 26 Silver has been well known for its antimicrobial characteristic. 27 So to overcome this problem silver nanoparticles are added in tissue conditioners because of their smaller size they provide large surface area.
Dental adhesives
Dental adhesives are the material used to promote adhesion or cohesion between two different substances or between a material and natural tooth structure. Polymerizable silane is added to dental adhesives in order to increase the cohesive strength. Since the adhesive liquid are not very viscous the filler particles tend to settle out during storage which leads to inconsistency in their performance. To overcome this disadvantage discrete silane treated nanoparticles of silica or zirconia in the size range of 5-7nm 28 are added to dental adhesives. According to a study by N. Silikas et al., no decrease in bond strength of dental adhesives after the incorporation of silica or zirconia nanoparticles was obtained. 29
Composites
Dental composite resins are types of synthetic resins which are used in dentistry as restorative material. Synthetic resins evolved as restorative materials since they were insoluble, aesthetic, insensitive to dehydration, easy to manipulate and reasonably inexpensive. 1. Nanofill Composites (Fig:2). Nanofills are the dental composites in which all the fillers are of 1-100 nm range. Two types of nanoparticles are used for preparing nanofill dental composite. 30 The first of these is the most common and are nanomeric particles which are essentially mono- dispersed non-aggregated and non-agglomerated particles of silica.
The second type of nanoparticle used to prepare nanofill composites is nanoclusters. This is done in order to overcome the disadvantages of the previously used nanomeric nanoparticle. Nanoclusters are made by lightly sintering nanomeric oxides to form clusters of a controlled particle size distribution. Nanoclusters from silica sols only 31 as well as from mixed oxides of silica and zirconia have been synthesized. 32
Nanohybrid Composites Prepolymerized organic fillers are incorporated so as to improve the undesirable rheological properties of composites where nanomers were included. 33
Titanium Di-Oxide Reinforced Resin Based Composites - According to study conducted by Yang Xia et al., titanium dioxide nanoparticles treated with organosilaneallyltriethoxysilane (ATES) are used in order to improve the microhardness and flexural strength of the resin based composites. 34 G. Polizos conducted a study in which titanium dioxide nanoparticles were synthesized in an aqueous solution. They were dispersed into an epoxy polymer matrix. The obtained material showed better mechanical properties. 35
Nanocomposite with Alumina Nanoparticles - According to study conducted by M. Al Haik et al., inclusion of alumina nanoparticles increases the hardness of the nanocomposite as compared to other nanocomposites. The production of alumina nanoparticles is done by using a low power plasma torch. 36 Zhanhu Guo et al., conducted a study in which alumina nanoparticles have been successfully functionalized with a bi-functional silane surfactant by a facile method. The result was significant increase in both modulus and strength. The addition of the functionalized nanoparticles has no deleterious effect on the thermal stability of the composite and the vinyl ester resin after curing has effectively protected the alumina nanoparticle from dissolution in both acidic and basic solutions.37
Dental porcelain
Dental porcelains currently used for ceramic restorations are brittle, and it is sometimes necessary to replace fractured or chipped restorations. Porcelain is fragile and exhibits elastic deformation rather than plastic deformation, leading to fracture or chipping of restorations.
The addition of silver nanoparticles significantly increased the fracture toughness and vickers hardness of the porcelain.34 Tokushifujieda et al., conducted a study in which they incorporated nanoparticles of precious metals of silver and platinum in dental porcelain and came to a conclusion that the addition of silver and platinum nanoparticles enhanced the mechanical properties of porcelain. The addition of silver and platinum nanoparticles increased both the Young’s modulus and the fracture toughness of dental porcelain. Silver nanoparticles increased the fracture toughness more than platinum.38
Gingiva gum shade aesthetic pink fine hybrid nano composite
It is used to treat cervical defects and exposed, discoloured or hypersensitive necks of teeth, especially in the visible anterior area. The gingival-like pink shades allow the correct reproduction of the gingiva. The system comprises 6 different flowable restoratives in VITA G1, G2, G3, G4, GOL, GOD shades plus 6 different fine hybrid, thicker consistency gingiva shaded composite restoratives in VITA G1, G2, G3, G4, GOL, GOD Shades. There is GC initial gum shade set.
Composition
1. Bis-GMA Urethane Dimethacrylate
2. Inorganic nano fillers
3. Ytterbium Fluoride
Implants
Dental implant therapy has been one of the most significant advances in dentistry in the past three decades. Osseointegration is widely accepted in clinical dentistry as the basis for dental implant success. Failure to achieve osseointegration can be attributed to one or more implant, local anatomic, local biologic, systemic or functional factors. 39, 40 Nanostructured hydroxyapatite coatings for implant have attracted attention during the last decade. Hydroxyapatite promotes bone formation around implant, increases osteoblasts function such as adhesion proliferation and mineralization. Nanoporous ceramic implant coatings use a different approach to improve implant properties, i.e. annodisation of aluminum. This technique was used to create a nanoporous aluminum layer on top of titanium alloy implants. 41 Nanoporous alumina has the potential of being rendered by loading the porous structure with appropriate bioactive agents improving cell response and facilitate osseoinductive activity. 42 Titanium and Titanium alloys are novels which have been successfully used as dental implants because these materials have good integration with adjacent bone surface without forming a fibrous tissue interface. For the optimization of bone growth, surface treatment has been applied such as surface roughening by sand blasting, hydroxyapatite coating, 43 formation of titanium dioxide or titania. 44
Nanosurface coatings
New coating technologies have also been developed for applying hydroxyapatite and related calcium phosphates (CaP), the mineral of bone onto the surface of implants. Many studies have demonstrated that these CaP coatings provided titanium implants with an osteoconductive surface. 45, 46 Following implantation, the dissolution of CaP coatings in the periimplant region increased ionic strength and saturation of blood leading to the precipitation of biological apatite nanocrystals onto the surface of implants. This biological apatite layer incorporates proteins and promotes the adhesion of osteoprogenitor cells that would produce the extracellular matrix of bone tissue. Furthermore, it has been also shown that osteoclasts, the bone resorbing cells, are able to degrade the CaP coatings through enzymatic ways and created resorption pits on the coated surface.46 Finally, the presence of CaP coatings on metals promotes an early Osseo integration of implants with a direct bone bonding as compared to non-coated surfaces. The challenge is to produce CaP coatings that would dissolve at a similar rate than bone apposition in order to get a direct bone contact on implant surfaces. Nano surface modifier's; Bone morphogenic proteins (BMP-2) increase osteoblast proliferation and embedded antiobiotics = supercharged bone growth.
Nano scale surface modifications
Surfaces properties play an important role in biological interactions. The nanometer sized roughness and the surface chemistry have a role in the interactions of surfaces with proteins and cells. These early interactions will in turn condition the late tissue integration. With these prospects in mind, different methods have been reported for enhancing bone healing around metal implants. 47, 48 Modifying surface roughness has been shown to enhance the bone-to-implant contact and improve their clinical performance. 47, 49 Grit blasting, anodisation, acid etching, chemical grafting, and ionic implantation were the most commonly used methods for modifying surface roughness of metal implants. Combinations of these techniques could be used such as acid etching after grit-blasting in order to eliminate the contamination by blasting residues on implant surfaces. This grit blasting residue may interfere with the osteointegration of the titanium dental implants.49, 50, 51 It has been shown that grit-blasting with biphasic calcium phosphate (BCP) ceramic particles gave a high average surface roughness and particle-free surfaces after acid etching of titanium implants. Studies conducted both in vitro and in vivo have shown that BCP grit-blasted surfaces promoted an early osteoblast differentiation and bone apposition as compared to mirror-polished or alumina grit-blasted titanium.52, 53 Anodisation is a method commonly used to obtain nanoscale oxides on metals including titanium 54, 55 By adjusting the anodization condition such as voltage, time, and shaking, nanoscale properties could be controlled.
Bone replacement materials
Bone is a natural nanostructured (i.e. a material with constituent features less than 100 nm in at least one dimension) composite composed of organic compounds (mainly collagen) reinforced with inorganic ones (HA). It is this natural nanostructure that nanotechnology aims to emulate for orthopedic and dental applications. 56 The smaller the particle is, the larger the surface area is in volume. Nano-Bone® uses this principle. The nano-crystallites show a loose microstructure, with nanopores situated between the crystallites. This material structure will be completed by pores in the micrometer area. By following this process, a rough surface area is formed on the boundary layer between the biomaterial and cell, which is very important for fast cell growth. Porosity values of around 60% can be found in both the nano and the micrometer pores. All pores are interconnecting (i.e. by being in contact with the patient’s blood, bodily substances merge into the pores). Because the cells are too big for the small pores, blood plasma containing all the important proteins is retained in the interstices. The surface of the pores (and also of the nanopores) is modified in such a way that it literally “hangs on” to the proteins. This is to be carried out by silica molecules. The compound silica is most important.
Tissue integration
The biological events occurring at the tissue-implant interface are influenced by the chemistry, topography, and wettability of dental implant surfaces. The challenge in developing new implant surface consists in increasing the clinical success rate as well as decreasing the tissue healing time for immediate loading of implants, particularly in aesthetic situations. 57, 58, 59 One of the objectives is to develop implant surface having predictable, controlled, and guided tissue healing.).
Effects of Nanoparticles
Nano toxicology is defined as a science that deals with adverse effects of engineered Nano devices and nanostructures in living organisms. Studies have shown significant association of increased cardiovascular mortality, other extra pulmonary effects, tissue damage, systemic effects due to increased rate of absorption of non-degradable nanoparticles by skin, lungs, etc. Silver nanoparticles are showing unacceptable toxic effect on human health and environment. The chronic exposure to silver causes adverse effects such as permanent bluish grey discoloration of skin (argyria) and eyes (argyrosis), liver and kidney damage.
Conclusion
The uses of various nanoparticles in acrylic resin, tissue conditioner, dental adhesives, composites, dental cements, dental porcelain, implants and maxillofacial prosthesis are discussed. However, further studies are required to clarify the cytotoxicity of various nanoparticles, optimal concentration and mechanical stability for proper and safe clinical experience. Following are the list of most suitable nanoparticle used in combination with different dental materials used in field of prosthodontics-
For acrylic resin - silver nanoparticles
For tissue conditioner - silver nanoparticles
For dental adhesives - silica or zirconia nanoparticles
For composites - titanium dioxide nanoparticles
For dental cements - silver nanoparticles
For dental porcelain - silver and platinum nanoparticles
For implants - nanostructured hydroxyapatite and Nano porous alumina
For maxillofacial prosthesis - silver, titanium dioxide and cerium dioxide nanoparticles.