- Visibility 82 Views
- Downloads 7 Downloads
- DOI 10.18231/j.aprd.2021.004
-
CrossMark
- Citation
Basal implants – A blessing for atrophied ridges
- Author Details:
-
Neha Pathania *
-
Harvinder Singh Gill
-
Archana Nagpal
-
Sharad Vaidya
-
Jenny Lalmalsawmi Sailo
Introduction
These days rrestoring the edentulous maxilla or mandible with implants has become an expected treatment. There should be sufficient bone available (at least 13-15mm length and 5-7 mm width)[1] for successful implant placement. Whenever the criteria is not followed properly then treatment planning for inserting implants becomes more difficult. There should be a need to restore the lost alveolar dimensions for a predictable successful outcome of the treatment. Such procedures include inlay or only alveolar grafts, nerve repositioning, sinus lift and even nasal lift, without which treatment with conventional implants might not be very successful.[2]
These surgical procedures also have their own indications and contraindications. The other attainable option for replacement in atrophic jaws is to change the implant design so that we can avoid these procedures. In the past few decades two rewarding implant designs and protocols have been revealed for restoring atrophic jaws that are Mini Dental Implants and Basal Implants.
Basal implants are dental implants that engage the highly dense cortical bone which has least propensity for resorption for implant retention. These implants are incomparable and designed for gaining anchorage from the basal cortical bone. The present time basal implant has a advanced design, surgical protocol and is a prosthetic favourable system. Due to these properties several practitioners around the world include basal implantology in their practices and so far these implants has given very desirable results.[3]
Crestal implantology is the most common implant standards these days where the implants are placed in the crestal alveoli of the jaw bone, and load trasmission ocur in vertical direction from their surfaces. They are available in the form of cover screws, cylinders, and blade implants. Usually the anterior mandibular has sufficient vertical bone heigh so the screw of 10-13 mm can be placed in this area. But this design cannot be put into practice in patients with severely resorbed mandibular ridges.Thus, the basal implantology was developed and it involves the placement of implants in the basal cortical bone, which provides excellent quality cortical bones for retention of these advanced implants. They are also known as cortical, or biocortical implant and by other terms such as orthopedic implants because they follow the rules of orthopedic surgery.[4], [5] They are also called as disk or lateral implants. The second major reason to use the basal cortical bone for these implants instead of the alveolar bone is the stress-bearing area of particular dental implant placement site can also be loaded with teeth immediately.[6] Basal implants provides multicortical support which gives absolute primary implant stability in dense living native bone.[7]
History
Basal implants have been developed and improved in several stages by majorly the German and French dentists. In 1972, Dr. Jean-Marc Julliet developed and used the first single piece implant, which has been used to this very day successfully, with only disadvantage of the lack of a surgical kit.[8], [9] In mid 1980s French dentist Dr. Gerard Scortecci improved the basal implant system with matching surgical tools and external and internal connections for the prosthetic superstructure; which he called “Diskimplants”.[9]
Based on the Dr. Gerard Scortecci’s Diskimplant, several German dentists have developed new implant systems and surgical tools, which gave rise to the development of the modern Basal Osseointegrated Implant (BOI), also known as “Lateral Implant”. These implants were designed to allow masticatory load transmission in the vertical as well as its basal part.[8], [9]
The manufacturing of lateral basal implants like the Diskimplants was started in 1997 by Dr. Stefan Ihde. These lateral implants had limited sizes and shapes and their surface was initially roughened. Soon he improved the basal implants; the round base plates got edges, preventing early rotation of the implants in the bone before integration. In 2002, in Europe and United States fracture proof base plate was invented and later patented also the bending zones in the vertical implant shaft were introduced. In 2005 screwable designs (BCS, GBC) were introduced.[8]
The vertical shaft surfaces were polished in 1999. The whole basal implant was produced with polished surfaces since 2003 (polished surfaces show no tendency to inflammation, and in case of sterile loosening, the implant-reintegration was possible if the load is adjusted well in time). Roughened osseous surfaces were lacking this ability. This design was developed to leave enough elasticity for the development and the functional bone stimulation.[8]
|
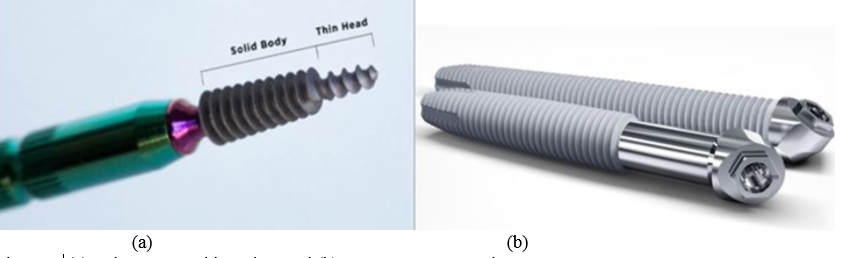
1. Screw form- Single Piece (monobloc) ([Figure 1]) |
A. Compression Screw Design{King Of Single Piece (KOS) Implant} B. Bicortical Screw Design (BCS Implant) C. Compression Screw + Bicortical Screw Design (KOS Plus Implant) |
|
2. Disk Form- Basal Osseointegrated Implant (BOI)/ Transosseous Implants(TOI) / Lateral Implant ([Figure 2]) |
A. According to abutment connection- a. Single Piece Implant b. External Threaded Connection c. Internal Threaded Connection- 1. External Hexagon 2. External Octagon B. According to basal plate design- a. Basal disks with angled edges b. Basal disks with flat edges also called as S - type implants. C. According to number of disks- a. Single disk b. Double disk c. Triple disk |
|
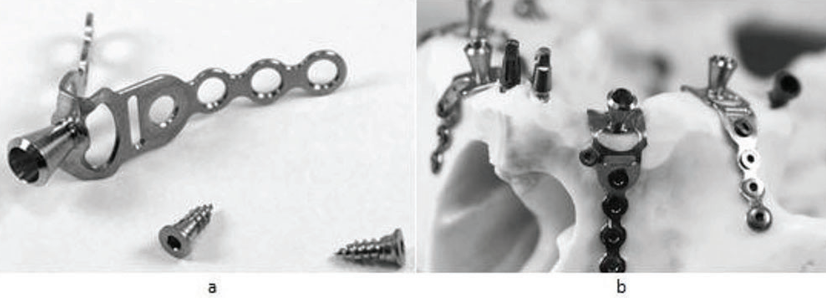
3.Plate form ([Figure 3])) |
A.Basal Osseointegrated Implant (BIO)-BAC Implant B. BOI-BAC 2 Implant. |
|
4.Other Forms([Figure 4]) |
A. Tuberopterygoid Implant(TPG) B. Zygoma Screw Implant(ZSI) |


Indications
Situations like several missing teeth or requiring extracted
Failure of 2-stage implant placement or bone augmentation procedure
All kinds of bone atrophies i e,
- Very thin ridge (high knife ridge, where crestal bucco-palatal bone thickness is < 2 mm; pencil mandible).
- Insufficient bone height. [11]
Contraindications
Heavy bruxism, clenching, uncontrolled malocclusion, and/or a history of fractured teeth, especially when associated with psychological problems.
High-dose IV bisphosphonates used in the treatment of severe osteoporosis or cancer (risk of osteonecrosis of the jaw). [11]
Facial and trigeminal neuropathies associated with a depressive state, epilepsy
Severe heart disease, recent stroke, or heart attack (risk of infective endocarditis), Uncontrolled diabetes , Untreated renal insufficiency.
Ongoing radiotherapy for cancer (risk of osteoradionecrosis of the jaw, especially after radiation of the head and neck region).
Age less than 15 years
Allergies or hypersensitivities to chemical ingredients of material used: titanium alloy (Ti6Al4V [6]
Certain diseases of the mucous membranes of the mouth,
An unbalanced relationship between the upper and lower teeth and Poor hygiene of the mouth and teeth
Infections in the neighboring teeth (pockets, cysts, granulomas , major sinusitis [11], [12]
Advantages of basal implants
Prosthesis is fixed within 72 hours of implant surgery saving time and costs considerably
Most of these implants take support from the basal bone which is a lot more resistant to resorption, Basal cortical bone also has a much faster and stable repairing capacity. [11]
There uniqueness in utilizing the available bone in the best possible manner to avoid bone augmentation procedures.
These implants work well in controlled diabetics, smokers and patients suffering from chronic destructive periodontitis. [12], [13]
Helps saving costs in a big way through avoidance of the bone grafts and second stage surgery, alongwith the phenomenal reduction in the total treatment time.
Basal implants have smooth surface, hence avoiding peri-implantitis [13]
Disadvantages of basal implants
Compromised aesthetics with single tooth replacement
Skilled surgeon with sound anatomic knowledge is required to carry out successful surgery [13], [14]
Excess sound bone reduction in cases of good bone support
Overload osteolysis can be seen, if load distribution is not done properly [14]
Surgery
Prior to surgery clinico-radiological examination of the patient has to be performed for determining the psychological and physical status of the patient. Special attention should be given to patients who have localized or systemic factors that could interfere with the healing process of bone, or soft tissue, or the osseo-integration process (e.g. smoking, poor oral hygiene, uncontrolled diabetes, facial radiotherapy, infections in neighborhood tooth or bone, patients passed bisphosphonate therapy). Pre-operative tissue (hard as well as soft) deficit may yield to compromised aesthetic result. [15]
The implant’s diameter, type, position and quantity should be selected individually taking the anatomy and spatial circumstances into account. Before implant treatments various tests should be done: Blood test, Mouth examination, X-ray examination, CT examination. [15]
Using local anaesthesia, the drills are used to create the implant bed. The implant is removed from the sterile pack and installed in the bone bed, immediately. Implants can be placed either manually with the ratchet or with a handpiece.
There is recommended Torque limitation provided for the basal implants: [15]
Basal implant from diameter 3 0 mm, via direct insertion - Never exceed 117 Ncm
Basal implant from diameter 4.5 mm - 5.0 mm, via direct insertion - Never exceed 238 Ncm
Basal implant from diameter 5 5 mm, via direct insertion - Never exceed 298 Ncm
Points to be considered prior to rehabilitating Atrophied maxilla and mandible:-
Mandible should be restored first because the stomato-gnathic system consists of stationery (maxillary bone) and a mobile (mandibular bone) component, the role of the mobile component is to apply forces and the stationery component absorbs a considerable amount of the forces applied. A conventional mandibular denture on an atrophied foundation is too unstable, leading to poor chewing function and later the associated muscles become atonic. [8]
For Atrophied Mandible
Two thoughts developed for implant restorations I atrophied mandible-
Multi-Implant Concept of French School [8](founded by Scortecci)According to this school basal and crestal implants are combined to form a rigid restoration, that does not permit any torsion across the mandible, also does not allow the jaw system to reorient forces.
Strategic Implant Positioning Concept of German School [4], [8] (founded by Dr. Ihde) According to this school four implants are placed in the mandible preferably in the canine and second molar regions, allowing the mandibular torsion and reorientation of forces which gets compensated by flexibility of the prosthesis, Thus avoiding the overload osteolysis and implant failure.
Infranerval Implantation Technique. [4], [16], [17]
In the atrophied mandible with advancing resorption the infra-alveolar nerve lies closer to the crest. The osteotomy prepared for the basal disk is prepared approx. 2-3 mm below the nerve, in an atrophied mandible. Thus, the basal disk gets inserted below the nerve, hence avoiding the need for extensive procedures.
For Atrophied Maxilla
Sinus Section Technique (SST)
The compression screw implants takes care of the porous bone, whereas, for the sinus two techniques have been described. In this two/three walls of the sinus are sectioned to facilitate placement of the basal disk in the sinus. The purpose is to gain bi-cortical support; also only one implant can be placed this way in each sinus. [8], [16]
Tuberopterygoid (TPG) Screws
These implants are inserted into the pterygoid bone and aid in providing additional support to the prosthesis.
These are used in combination with SST and are placed at 20º-45º in the bone and the angulation between BOI implant. Prosthesis placement becomes difficult, if TPG screws exceed 90º.[8]
Zygomatic Screw Implant (ZSI)
These zygomatic implants are placed in the zygomatic bone and have sharp edged cortical screws to gain bicortical support like the BCS implants. [16]
Peri-Implant Healing
Due to their special design, their peri-implant healing is also special. The skeletal bone remaining after tooth loss and complete resorption of the alveolar crest is termed Basal bone. This bone structure has a very low turnover (ten times less than alveolar bone) [12], [18] and is highly sensitive to thermal injury and infection.The main source of blood in atrophic jaws is the inner layer of the periosteum, hence the maintenance of aseptic conditions during surgery, careful handling of the periosteum, profuse saline irrigation during lateral osteotomy, and primary stability are of utmost importance in bone healing after basal implant installation. [12], [18]
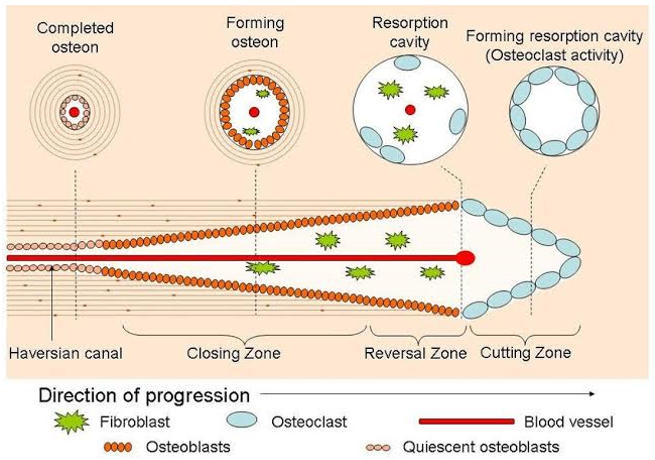
“Osseointegration” is the term used for conventional implant but the term “Osseoadaptation” [3] is the term used for basal implants because bone with continuous functional loads remodels and finally adapts over the surface of the implant. According to the philosophy of basal implantology the process of Osseoadaptation is carried out by a “Bone Multicellular Unit” (BMU), [8], [4] which forms when the BOI and BCS implants are subjected to immediate loading, further leading to remodeling of bone under functional stresses, finally forming tthe BMU unit, and thus initiates the healing phase and leads to formation of a dense peri-implant bone. [8], [4] Basal implants employ the same principles of peri-implant healing and bone densification, so they are also termed as “orthopedic implants”.
Healing process involves the following steps ([Figure 5]). [3]
Activation phase
In this phase, lasting for three days, the precursor cells/human mesenchymal stem cells develop into osteoblasts and osteoclasts. .
Resorption phase
In this phase, osteoclastic activity (occuring at the rate 40µm/day) shows soft and porous bone.
Reversal phase
In this phase, the osteoblastic activity occurs, where the osteoblasts lay down new bone in the haversian canals at a rate of 1-2µm/day.
.
Progressive phase
In this phase, the osteoblasts forms concentric lamella in haversian canals, which leads to reduction in diameter of the canal and increase in bone density. At this stage the diameter of the haversian canal is 40-50µm. Non-Mineralized Matrix Osteoid is the newly formed bone and this phase lasts for 3 months.
Mineralization phase
This phase begins after ten days of osteoid formation.
This phase involves two stages
Primary Mineralization Stage - imparts primary hardness to the osteoid and accounts for 60% of all mineralization.
Secondary Mineralization Stage - imparts final hardness and final morphology of bone. This phase lasts for 6-12 months.
Dormant phase
During this phase, osteocytes develop from osteoblasts and line the haversian canals and perform the mechanical, metabolic and homeostatic functions.
Throughout these phases the implants are under functional loads, leading to continuous stimulation of the BMU throughout the life of the implant, which increases the peri-implant bone density (which increases throughout the implants life) and to adapt over the surface of the implant, which is called “Osseoadaptation”.[8]
Side effects and complications with Basal implants
Activities demanding considerable physical exertion must be avoided, immediately after the insertion of dental implants.
Possible complications following the insertion of dental implants are
Temporary symptoms are pain, swelling, phonetic difficulty and inflammation of the gingiva.
More persistent symptoms are chronic pain in connection with implants, permanent paraesthesia, dysesthesia, loss of maxillary / mandibular ridge bone, localized or systemic infections, oro-antral or oro-nasal fistulae, unfavourably affected adjacent teeth, implant fracture , jaw / bone / prosthesis / aesthetic problems, nerve damage, exfoliation, hyperplasia. [15], [19]
Conclusion
Basal implantology is a new treatment strategy `with new broad indications and almost no limitations. Unlike the traditional concepts in oral implantology, the basal implantology does not include any bone build-up procedures for the subsequent installation of implants. Additionaly, it offers advantages like the flapless approach with minimal surgical effort (thin mucosal penetration) reduced post-operative pain, avoid any swelling and reduce the discomfort. [20]
They can be used to bypass the mandibular nerve in the mandible and for engagement of the cortical bone at the fusion of the pterygoid with the maxilla.The direction of abutments are adjustab up to 15° relative to the implant axis. Also with respect to the accepted principle “primum nihil nocere”,[21] i.e., limiting treatment, basal implants are the devices of first choice, whenever (unpredictable) augmentations are part of an alternative treatment plan. In an atrophied mandibular alveolar ridge, using the basal implants for the restoration of function is an effective alternative to the use of conventional implant techniques. These implants pose no risk for moderate loading after immediate insertion of the implants.[6]
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- S Ihde. Restoration of the Atrophied Mandible Using Basal Osseointegrated Implants and Fixed Prosthetic Superstructures. Implant Dent 2001. [Google Scholar] [Crossref]
- R Sharma, Jai P, A Dhruv, A Hasti. Basal Implants- An Alternate Treatment Modality for Atrophied Ridges. IJRID 2016. [Google Scholar]
- A D Gupta, A Verma, T Dubey. Saloni Thakur Basal Osseointegrated Implants: Classification and Review International Journal of. Contemp Med Res 2017. [Google Scholar]
- S Ihde. Comparison of basal and crestal implants and their modus of application. Smile Dent J 2009. [Google Scholar]
- DR Carter, DM Spengler. Mechanical Properties and Composition of Cortical Bone. Clin Orthop Relat Res 1978. [Google Scholar] [Crossref]
- Tha TP, D Ganapathy, AR Jain. Basal implants - A review. Drug Invention Today 2018. [Google Scholar]
- G M Scortecci. Basal Implantology. . [Google Scholar]
- I Stefan. Principles of BOI- Clinical, Scientific, and Practical Guidelines to 4-D Dental Implantology. 2005. [Google Scholar]
- Y Babita, N Choudhary, B Nazish, T Gaurav, K Pranit. Basal Osseointegrated Implants. IJAHS 2016. [Google Scholar]
- A D Gupta, A Verma, T Dubey. Saloni Thakur Basal Osseointegrated Implants: Classification and Review. Int J Contemp Med Res 2017. [Google Scholar]
- . Disadvantages of basal implants. 2015. [Google Scholar]
- G M Scortecci. . Basal Implantology.ISBN . [Google Scholar]
- . Advantages of immediate loading basal implants. 2015. [Google Scholar]
- Grishmi Niswade, Mitul Mishra. Basal Implants- A Remedy For Resorbed Ridges . WJPLS 2017. [Google Scholar]
- . Insruction for use dental implant system ROOTT BASAL and BASAL SS implants. . [Google Scholar]
- A David, F Ghazaei. Case Description of a New Graftless Solution for a Patient with Complete Alveolar Ridge Loss in the Molar Part of the Maxilla. Presented at Polish Association of Implantologists. 2013. [Google Scholar]
- F Ghazaei, F Spahn. Treatment Concept for Extremely Atrophic Mandibula Renouncing on Grafts and Heavy Surgery in Bone Heights of Less than 5mm. 2014. [Google Scholar]
- D Henri. Immediate Loading of a Maxillary Full Arch Rehabilitation Supported by Basal and Crestal Implants. Adv Dent and Oral Health 2008. [Google Scholar]
- O Ahmad, B Thamer. Basal screw implantology without sinus lifting. Pak Oral Dent J 2014. [Google Scholar]
- A Otoum. Master of Immediate Loading Thamer Bsoul, Bds, Jdbbasal Screw Implantology Without Sinus Lifting. Pak Oral Dent J 2014. [Google Scholar]
- R S Yadav, R Sangur, T Mahajan, A V Rajanikant, N Singh. Singh RAn Alternative to Conventional Dental Implants: Basal ImplantsRama Univ. J Dent Sci 2015. [Google Scholar]
