Introduction
The goal of modern dentistry is to restore the patient to normal contour, function, comfort, esthetics, speech, and health. As a result of continued research, diagnostic tools, treatment planning, techniques and materials Implant dentistry is able to achieve this goal with predictable success.1 Compared with traditional methods of tooth replacement, the implant prosthesis offers increased longevity, improved function, bone preservation, and better psychological results.2
But installation of the implants requires the remaining alveolar ridge to have adequate height and thickness, so that the implant ideally possesses 1.5mm of bone tissue along its entire circumference.3 This problem is especially magnified in the posterior maxilla, where progressive ridge resorption in an apical direction is combined to the progressive sinus pneumatization as a consequence of intrasinus positive pressure.4 In addition to the residual alveolar bone resorption, the maxillary sinus expands after tooth loss. As a result, the available bone height is decreased from both the crestal and apical regions. To overcome these problems, different solutions were proposed over the years, such as the use of short implants, tilted implants placed in the anterior maxilla, zygoma implants, and maxillary sinus floor elevation and grafting procedures with autogenous bone or allografts, xenografts, and alloplastic materials. Reports of high failure rates of short implants (8mm or less) placed in the posterior maxilla led to recommendations that a minimum implant length of 10 mm, with a diameter of between 3 and 4 mm, is necessary to guarantee the long-term success of implants, particularly in the maxilla, where the bone quality is generally poorer than in the mandible. This often required sinus floor elevation and grafting. This procedure involves placing bone-graft material in the maxillary sinus to increase the height and width of the alveolus.5
In this article we will be discussing in detail the various anatomical and clinical considerations in the posterior maxillae for sinus floor elevation procedure to ensure a predictable success with minimum complication.
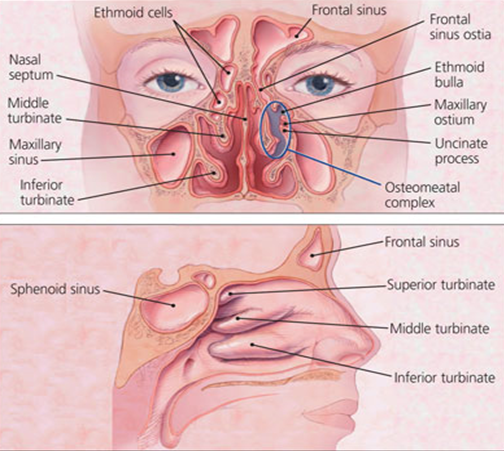
Anatomy of maxillary SINUS
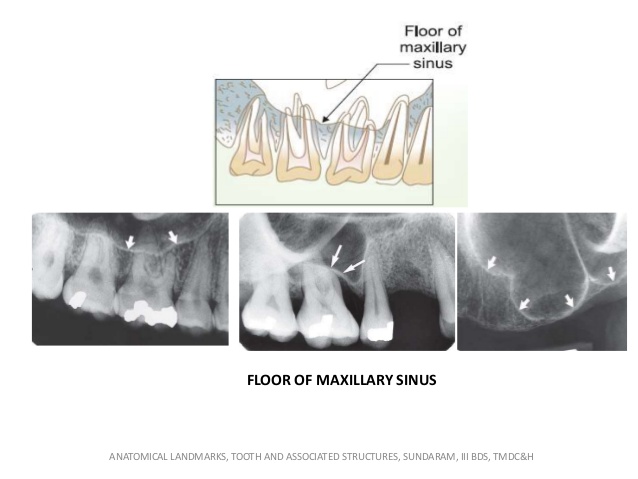
The in-depth knowledge of anatomy of the maxillary sinus is utmost important before actually performing the sinus floor elevation procedure. 6 In the middle ages, during the Renaissance, Leonardo da Vinci and Andreas Vesalius both described the paranasal sinuses, including the maxillary sinus, in great detail. The maxillary sinuses were first illustrated and described by Leonardo da Vinci in 1489 and later documented by Nathaniel Highmore in 1651.7 The maxillary sinus or Antrum of Highmore lies within the body of the maxillary bone and is the largest and first to develop of the paranasal sinuses. The average dimensions of the maxillary sinus are 36–45 mm in height, 23–25 mm in width, and 38–45 mm in length (anteroposterior axis).8 The maxillary sinus is a pyramid-shaped cavity occupying the body of the maxilla which contains roughly 12-15ml of air. Inferior portion of the sinus is typically 1 cm below the nasal floor. Its apex extends to the zygomatic process of the maxilla (processus zygomaticus), while its baseline forms part of the medial wall of the maxillary sinus and the lateral wall of the nasal cavity. The pyramid has three main processes or projections: (1) the alveolar process inferiorly (bounded by the alveolar ridge), (2) the zygomatic recess (bounded by the zygomatic bone), and (3) the infraorbital process pointing superiorly (bounded by the bony floor of the orbit, and below it, the canine fossa). The alveolar and palatine processes form the floor of the maxillary sinus, which after the age of 16 usually lies 1–1.2 cm below the floor of the nasal cavity.
The anterior wall of the sinus extends from the inferior orbital rim to the maxillary alveolar process and contains infraorbital neurovascular bundle.
Superior wall is very thin floor of the orbit. Posterior wall separates maxillary sinus from pterygopalatine fossa which contains posterior superior alveolar nerve and blood vessels, the pterygoid plexus of veins and internal maxillary artery. Medial wall is the lateral wall of the nasal cavity and also houses primary ostium that serves as the main channel for the drainage of secretions. And last is the Lateral wall forming the buccal aspect of the sinus and serves as an access route for direct sinus lift or the lateral wall sinus graft procedure.9
The Ostium
The sinus drains medially and superiorly into the nasal cavity via the ostium. The ostium size can vary from 1 to17 mm and averages 2.4 mm. The medial wall houses the primary ostium, which serves as the main conduit for drainage of secretions. The natural ostium is located in an anteromedial position in the superior aspect of the medial sinus wall (lateral nasal wall), and its location makes sinus drainage by gravity impossible.10 It drains into the ethmoidal infundibulum, then into the middle meatus of the nasal cavity at the hiatus semilunaris. It opens into the semilunar hiatus of the nasal cavity and is usually located in the posterior half of the ethmoid infundibulum behind the lower one-third of the uncinate process. Accessory ostia are found in approximately 15% to 40% of patients.11 They typically drain superior to the inferior turbinate, superior and posterior to the uncinate process. The ostium of the maxillary sinus is on the highest part of the medial wall of the sinus and inflammation of which can interfere with drainage. 10 11
Schneiderian Membrane
The maxillary sinus bony cavity is lined with the sinus membrane, also known as the Schneiderian membrane. This membrane consists of ciliated epithelium like the rest of the respiratory tract. It is continuous with the nasal epithelium through the ostium in the middle meatus. The sinus linings, although similar in structure, are somewhat thinner than the lining of the nasal cavity. The Schneiderian (mucous) membrane lines the inner walls of the sinus and in turn is covered by pseudostratified columnar ciliated epithelium. The schneiderian membrane is composed of 3 layers. The first layer is periosteum, which covers the bone of the antrum. A layer of highly vascular connective tissue covers the periosteum. The last layer is pseudostratified columnar epithelium (respiratory epithelium) and is exposed to the sinus cavity.12 The Schneiderian membrane is approximately 0.8 mm thick in the antrum and the thickness varies from 0.5 mm to 0.13 mm. However, inflammation or allergic phenomena may cause it to thicken, either generally or locally. Since the most frequent surgical complication occurring during sinus augmentation is perforation of the Schneiderian membrane (10%-56%), it is crucial to check
the status of Scheniderian membrane by cone beam computed tomography or with an endoscope, and to eliminate sinusitis and other potential pathological conditions before any surgery.13 Chances of sinus membrane perforation depend
on the angle between the lateral and the medial wall of the sinus. Greater than 60º angle has 0% chances of perforation; narrow angles result in higher perforations.14
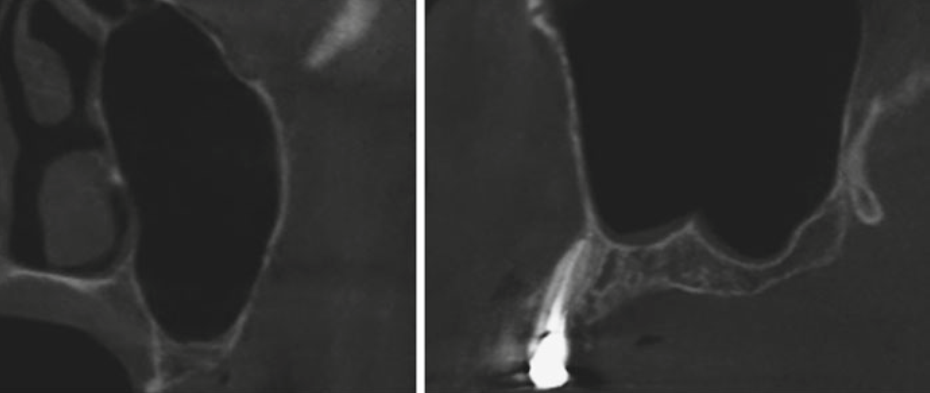
Bony septa of maxillary sinus
Maxillary sinus septa were first mentioned by Underwood in 1910. Maxillary sinus septa are barriers of cortical bone that divide the maxillary sinus into multiple compartments also termed as recesses.15 Diagnosis of presence of septa by computed tomography is important for planning maxillary sinus elevation surgery and later separating the sinus membrane from the septa.16 Septa have become increasingly important in maxillary sinus anatomy as surgical technique has developed. They may even occasionally reach from the base to the upper sinus wall, creating two sinuses. Based on their origin, Septa can be further subdivided into primary septa, formed during maxillary development and tooth growth, or secondary septum which is acquired during the pneumatization of the maxillary sinus after tooth loss. The majority of septa are located between the second premolar and first molar area.17 The formation of Underwood’s septa may be linked to the fact that teeth are lost at different times. The edentulous areas may resorb in a manner those results in a difference in level between the two adjacent portions of the sinus floor. It is thought that a bony septum may form in the area between the two regressing areas in order to transfer masticatory loads optimally. After the complete loss of teeth, the septa sometimes gradually disappear. Diagnosis using two-dimensional panoramic radiographs yields incorrect results in 29% of cases, and it has been suggested that three-dimensional computed tomography may be used to avoid complications during sinus augmentation.18 The septum has been related to increased risk of perforation of the membrane during sinus augmentation. The lateral window design may be modified by the making of two windows or one w-shape window if the septum is lowered. Septa may be cut with a chisel and be removed so that the graft can be placed without interruption. 19
Blood supply and nerve supply
The maxillary sinus is embedded in numerous anastomoses of various arteries receiving blood supply; the superior alveolar arteries (through the tuberosity), the greater palatine artery (posterior and medial wall), the sphenopalatine artery, the pterygopalatine, the infraorbital artery in the anterior wall and posterior lateral nasal artery in the medial wall.20 The anatomical course of the anterior maxillary wall and the alveolar process arteries is essential for sinus lift procedures. During these surgeries certain intraosseous vessels may be cut, causing bleeding complications in approximately 20 % of osteotomies.21 The venous system is collected either by a single trunk, which is a continuation of the sphenopalatine vein, or by three venous plexuses: the anterior and posterior pterygoid plexuses, and the alveolar plexus. The anterior and posterior pterygoid plexuses converge through the lateral pterygoid muscle and connect with the alveolar plexus, which drains partly into the maxillary vein and partly into the facial vein. 21
Sensory innervation of the maxillary sinus is supplied by the maxillary division of the trigeminal nerve (V-2) and its branches: the posterior superior alveolar nerve, anterior superior alveolar nerve, infraorbital nerve, and greater palatine nerve. The middle superior alveolar nerve contributes to secondary mucosal innervation. The natural ostium receives its innervation via the greater palatine nerve, and the infundibulum is supplied by the anterior ethmoidal branch of ophthalmic nerve (V-1). The mucous membranes receive their Post ganglionic parasympathetic innervation for mucous secretion from the greater petrosal nerve (a branch of the facial nerve).22
Lateral wall of maxillary sinus has two types of anastomoses one is in the buccal tissue which is called extraosseus and the other is within the buccal bony plate also called intraosseus anastomosis that occurs between infraorbital artery and posterior superior alveolar artery sometimes. Extraosseus anastomoses is 23-26 mm from alveolar ridge while intaosseus is 16-19 mm from the ridge, which can cause haemorrhage during flap elevation or window preparation through bone. It may appear as radiolucency in the sections of CBCT scan and has to be taken care of during procedure.23
Indications and contraindications
The indications for maxillary sinus floor elevation procedure are:
Severely atrophic edentulous maxilla
Insufficient residual bone height (RBH< 10 mm
Poor quality and quantity of bone available in posterior maxilla
Absence of any pathology in posterior maxilla and maxillary sinus
Local contraindications fall into two main groups: (1) potentially reversible (relative); and (2) irreversible (absolute). The first group includes pathologies that, if not treated, contraindicate sinus grafting. The second group includes pathologies that, even after surgical management, leave irreversible dysfunction of the osteometal complex.
Potentially reversible, relative contraindications to sinus grafting
Narrowing of the osteomeatal complex due to a deviated septum; abnormal morphology of the middle turbinate; medial or lateral rotation of the uncinate process or post-traumatic or postsurgical scarring.
Benign tumors of the nasomaxillary complex such as papillomas, schwannomas, osteomas, polyps, or mucus retention cysts.
Viral, bacterial, and micotic rhinosinusitis
Malignancy of the nasomaxillary region
Treatment of the offending etiology (eg, endodontic treatment of necrotic teeth, medical or surgical therapy of sinusitis, removal of tumors or polyps) must eradicate the pathologic condition prior to sinus graft augmentation.
Irreversible, absolute contraindications to sinus grafting
Some anatomic and/or structural alterations or pathologies of the nasomaxillary complex may represent absolute contraindications to the sinus graft procedure. These include:
Severe (uncorrected deformities of the maxillary sinus
Scarred and hypofunctional sinus mucosa following trauma or previous operation
Radiotherapy of the head and neck area (radiation dose above 45 Gy60
Chronic recurrent sinusitis, with or without polyposis that disrupts mucociliary clearance and is unresponsive to medical or surgical treatment
5. Local expression of a systemic granulomatous disease such as Wegener granulomatosis or midline idiopathic granuloma
Sarcoidosis
Benign but locally aggressive tumor (eg, ameloblastoma, myxoma, desmoplastic fibroma, inverted papilloma
Malignant tumor, both primary and metastatic, deriving from epithelial, connective, or odontogenic tissues 24
The following conditions, unless treated and under control with the patient's complete understanding of the risks, generally contraindicate the sinus graft procedure:
Chronic renal disease
Chronic liver disease
Uncontrolled diabetes
Uncontrolled hypertension
Myocardial infarction
Haemophilia or treatment with anticoagulant therapy
Metabolic bone disorders
Uncontrolled thyroid disorders
Uncontrolled adrenal disorders
Autoimmune diseases, including HIV
Steroid treatment at the time of the sinus graft procedure
Pregnancy
General Surgical Contraindications Include
Chemotherapy for the treatment of malignant tumors at the time of the sinus graft procedure
Radiotherapy
Drug or alcohol abuse
Heavy smoking
Physical or psychiatric handicaps
Patient noncompliance
Overall, absolute and relative contraindications for the sinus bone graft procedure take into account systemic manifestations of disease as well as local pathophysiology.25
Clinical and radiological assessment
Medical Evaluation
A thorough history, physical and dental examination is required before the initiation of treatment. The patient’s current medications as well as allergies should be reviewed. Appropriate laboratory investigations should be done when required and patient should be sent for the physician’s consultation as needed.
It may be judicious to ask for an ENT clearance in patients with chronic recurrent paranasal sinusitis. Some patients may even require functional endoscopic sinus surgery (FESS) to aid spontaneous drainage of the sinuses. Clinicians can use components of the sinonasal outcome test (SNOT-22) to predict likelihood of symptom improvement after surgical intervention. Nasal obstruction symptom evaluation (NOSE) test may be used by clinicians to assess possible areas of concern that may pose a threat to postoperative development of acute or chronic maxillary sinusitis. Both these are relatively simple methods of evaluation and may be used on an outpatient basis.26
Dental Evaluation
A comprehensive dental evaluation determines whether the patient is an appropriate candidate for implant placement with sinus augmentation. Diagnostic models can be used to evaluate the proposed surgical site. The patient’s occlusal scheme should be evaluated. In addition to horizontal measurements, the vertical dimension of the surgical site, the transverse relationship of the maxilla and mandible should be evaluated. An inadequate or excessive interarch distance can compromise the stability or esthetic outcome of the implants.27
Radiographic Evaluation
With moderately invasive surgical techniques such as sinus floor elevation (SFE) procedures, a defined clinical and radiographic diagnosis is always required to perform the procedure conveniently and with minimum complications. Currently, periapical (IOPA) and panoramic (OPG) X- rays are the most common initial dental radiographs for complete visualization of the maxillary sinus and evaluation of the remaining alveolar bone. 28
Periapical Or IOPA X-Ray
Periapical radiographs are usually selected to assess the residual bone height for the evaluation of sinus augmentation, examination of sinus proximity during indirect sinus augmentation, verification of implant osseointegration after implant placement, confirmation of implant-abutment seating before loading, and longitudinal assessment of peri-implant bone changes after loading.29
Panoramic OR OPG X-RAY
The panoramic radiograph shows both maxillary sinuses, revealing larger internal structure than the periapical image and parts of the inferior, posterior, and anteromedial walls. It is considered that panoramic image does not allow reliable or complete radiological representation of the maxillary sinuses even if it is the starting point of every sinus examination.30
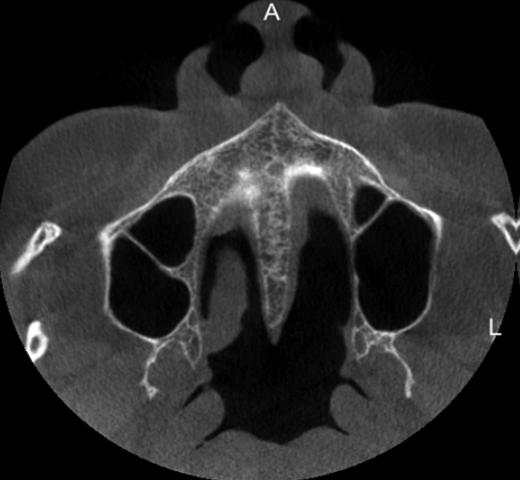
Computed tomography and cone beam computed tomography
Although CT is considered as the “gold standard” in imaging for visualization of the maxillary sinus, since the late 1990s, cone beam computed tomography (CBCT) is gaining increasing popularity in this respect. In implant dentistry, recent guidelines recommend the use of CBCT for three-dimensional treatment planning, especially prior to SFE – for evaluating both residual alveolar and sinus conditions.31 When a sinus lift procedure is planned the question arises, what we have to look for in CBCT or CT of the patient?
A Normal sinus will appear as a low-density homogenous cavity.
It is always suggested to extend the FOV to include the osteomeatal complex as it avoids postoperative complications resulting from a compromised drainage system. 32
If any bony septa is found in the maxillary sinus then removing with a chisel or haemostat is recommended or the technique is need to be modified accordingly when the septum is long or complete two different entries are recommended considering the maxillary sinus as two different cavities.
The design of the window preparation for direct sinus lift has to be modified according to height, location and diameter of the posterior superior alveolar artery and infraorbital artery.
Normally, the thickness of the Schneiderian membrane varies from 0.13 to 0.5 mm. However, inflammation or allergic phenomena may cause its thickening, either generally or locally. It is generally associated with some kind of irritation, such as odontogenic pathology or allergic phenomena.
The last dimension which is required to be recorded through CBCT is Residual Bone Volume which is a total of Residual Bone Height (RBH) and Residual Bone Width (RBW). Sinus floor elevation is generally recommended when RBH < 4-6 mm. 33
The Report of the Sinus Consensus Conference of 199610 noticeably stated that in a class A situation (i.e. RBH > 10 mm), conventional implant protocol could be followed. When the case is class B scenario (i.e. RBH < 7 mm to 9 mm), simultaneous implant placement and indirect sinus floor elevation through crestal approach could be done. In case of a class C patient (4 mm to 6 mm residual bone height), a lateral approach involving a grafting material with immediate or delayed implants is generally advised. Finally, with a class D patient (1 mm to 3 mm residual bone height), a lateral approach involving a bone grafting material and delayed implant placement is advocated. 34
Conclusion
Sinus lift surgery is an established and reliable technique because of the low rate of postoperative complications and the success of implants placed in the grafted area. However, as with any surgical procedure, it is not immune from risk. To minimize this risk, the surgery must be carried out by experienced professionals with appropriate planning. The major part of success with implant
Placement in posterior maxilla by grafting procedure lies in treatment planning. It is of paramount importance that the preoperative evaluations are performed perfectly and the most suitable technique is decided wisely for that particular situation, to improve the prognosis of that treatment. In this report we have discussed in detail the anatomical relations of maxillary sinus, preoperative evaluation, diagnosis and treatment planning before performing the actual sinus floor elevation surgical procedure. These findings can be helpful in skilfully performing the procedure with minimum complications and morbidity and maximum success rates and excellent prognosis.