Introduction
The ever-increasing speed of life puts forth a need to improve the effectiveness of the rehabilitative procedures and other interventions we perform on our patients. This improvement is primarily focused on simplifying the procedures, reducing the number and extent of interventions, reducing the time taken for treatment, maintaining, and improving the durability and quality of the rehabilitation without compromising on patient safety. The contemporary mainstay of management of edentulous patients is either a removable denture, fixed bridge or conventional / crestal / rough surface two-piece implant based fixed prosthesis depending on the suitability of the patient, affordability, and expertise of the operator. All these treatment modalities are fraught with limitations in terms of comfort, effectiveness, durability, violation of the abutment tooth structure and time taken for completion of the treatment.1, 2 Since the implant-based replacement of the missing tooth / teeth is the contemporary standard of care there has been a continuous endeavour to improve the clinical outcome in the minimum time possible. However, owing to its surface characteristics and design the conventional implants have a severe limitation with regards to complexity of the procedure, multiple steps and components and time taken for completion of treatment. Additionally, these often require a plethora of adjunctive procedures for management of difficult cases,3, 4 thereby making the conventional implants susceptible to failure due to peri-implantitis and other causes.4, 5 Although there are different kinds of basal / corticobasal / immediate loading implants available in the market by different manufacturers, in our study we used the BECES implant. Its a polished surface, single piece Strategic Corticobasal Implant (SCI) composed of Ti6AI4V ELI alloy manufactured by Ihde Dental, Germany [Figure 1]. This implant very successfully offers a treatment option which is remarkably simple, effective, durable and completely obviates the need of adjunctive procedures thus enabling the operator to effectively
manage any given edentulous situation in a significantly shorter duration of total treatment time.6 These implants are available in various combinations of diameter and length ranging from 2.7 mm to 12 mm diameter and 8 mm to 55 mm length. In contrast to the conventional two stage rough surface implantology, in which the implants placed derive anchorage / stability from the cancellous bone of the residual alveolar ridge, the SCI is placed in resorption stable basal / cortical bone and immediately loaded with a prosthesis in functional occlusion thereby reducing treatment time from 3 - 6 months taken for conventional implantology, to 3 - 6 days by SCI. Our study was targeted at assessing the versatility of these SCI in various clinical scenarios.
Aim
To assess the effectiveness of the strategic corticobasal BECES implant in the management of various edentulous cases.
Objectives
To assess the utility of various imaging modalities in the treatment planning and post-operative follow-up.
To assess the versatility if the BECES implant in various clinical situations
To assess the sacrosanct rigidity of the 72-hour loading protocol
To assess the need of adjunctive procedure like sinus lift, bone and or soft tissue grafting.
To compare the clinical results vis-à-vis standard published data on conventional implantology
Materials and Methods
This longitudinal observational study was carried out at our centre from Mar 2017 to Feb 2018. Patients reporting to the Outpatient Department (OPD) requiring tooth replacement were included in the study. However poor general health condition, terminally ill patients, patients with oral cancers, radiation therapy, ongoing / recently completed chemotherapy, patients on or after bisphosphonate therapy and or Medication related osteonecrosis of the jaw (MRONJ), oromandibular dystonia, patients with conditions like Cerebral Palsy, Parkinson’s etc who were unfit for implant placement under local anaesthesia and or unable to cooperate for other steps of prosthesis fabrication were excluded from the study. Additionally, patients who were unable to commit attendance for recall visits as per the protocol at 1,3,6,12 months and yearly review thereafter were excluded. Apart from these, all other patients were included in the study irrespective of their comorbidity status. Their medical conditions like Diabetes, Hypertension, Heart disease etc were optimized as per standard surgical protocol and taken up for implant placement and subsequent fabrication and placement of prosthesis. Smokers were counselled to discontinue the habit. Oral prophylaxis and extraction of impacted teeth was carried out in all patients as a preoperative protocol in partially edentulous cases. Necessary Institutional Review Board approvals and patient consent were obtained prior to the procedure.
Immediate functional loading protocol
As per the recommendations of the consensus group, the SCI are to be functionally loaded with in 72 hours of implant placement in the patient’s mouth.6, 7 This recommendation is based on the premise that subsequent to the osteotomy the bone shows increased osteoclastic activity with initiation of osteonal remodelling after approximately 72 hours, which may be detrimental to the stability of the implants. Therefore, it is advised that the prosthesis to be placed and occlusion adjusted prior to the initiation of this remodelling activity. The prosthesis with rigid framework, placed early, provides a splinting effect, thus providing better stability and resistance to occlusal load during the osteoclastic and subsequent healing in phase of the treatment.
Treatment planning & execution
The steps followed in rehabilitation of a complete edentulous case with SCI were as follows:
Clinical examination and diagnostic radiographs
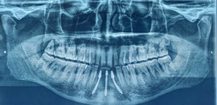
Orthopantomogram (OPG) was done as a protocol for planning of the implant sites and assessment of the jaw bones. The implant sizes were estimated based on the OPG image and empirical judgement. Cone beam computerized tomography (CBCT) was resorted to only in cases where the diagnostic information required was insufficiently available from the OPG. Since these implants derive primary anchorage from the second / third cortical bone, the quality and quantity of the alveolar bone is inconsequential.8 Additionally, the polished surface of these implants makes them conducive to trans-antral placement, thus obviating the need for adjunctive procedure of any sort. Also, owing to the bendability, the Inferior Alveolar Nerve (IAN) can be bypassed without any special consideration regarding the size of the implant.9
Type of implant
In our study the BECES [Figure 1 ] implant was used. It is a polished surface, single piece implant. The BECES implant by virtue of its design gains anchorage at the apical portion of the implant and can be used in all areas of the complete / partially edentulous jaws [Fig 1]. In our study we have used BECES implants in Full Mouth Rehabilitation (FMR) and segment reconstruction cases in all regions of the mouth. Although the implant is very versatile, its placement is highly technique sensitive especially when being used in the pterygoid region. In experienced hands the BECES implant suffices in all edentulous areas, as it can be anchored in the second / third cortical bone and the implant head can be bent to make it parallel with the adjoining implant / tooth to receive a prosthesis.
Number of implants
The number of implants indicated / used in our study were as follows:
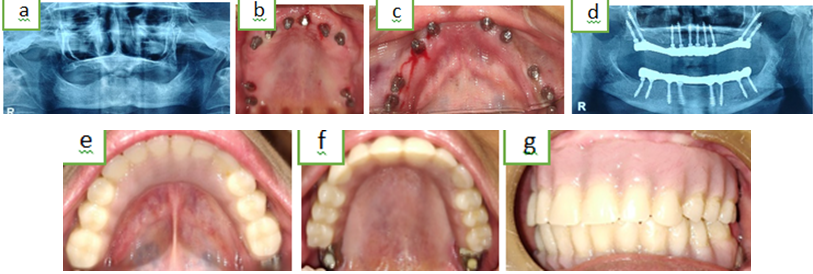
In an FMR case 10 implants in the maxilla and 08 in the mandible were placed as per the supporting polygon recommendations of the consensus group. 6, 7, 10, 11 Of these, 06 implants were placed in the anterior maxilla between the inter-canine region and a double pterygoid on either side in the molar region. In the mandible, 04 implants were placed in the inter-foramina region and two in the molar region on either side [Figure 4]. Where indicated, a single Zygoma / ZDI implant was used in each side of the maxillary arch along with the 08 other implants in the maxilla i.e. 06 implants in the inter-canine region, one zygoma on each side and on pterygoid on each side.[Figure 19].
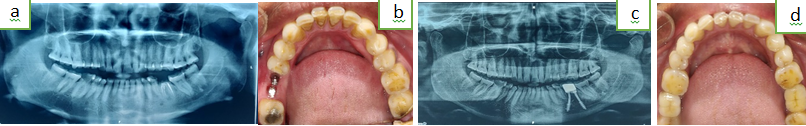
For segment reconstruction involving more than one posterior tooth a minimum of one additional implant was placed in addition to the total number of teeth being replaced [Figure 10, Figure 12, Figure 21 d].
For single premolar in the maxilla one / two implants were used depending on the available bone and the space available for of the implants [Figure 14, Figure 18]. Similarly, for a single maxillary molar, two / three implants were placed [Figure 16, Figure 18, Figure 24 ].
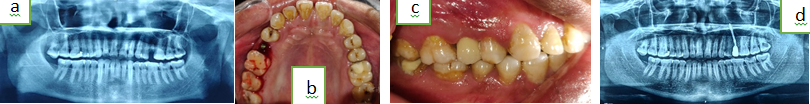
In the mandible, the premolars were replaced using a single implant, however for a single molar, two implants were used [Figure 5, Figure 13, Figure 23].
The incisor in both arches was replaced using a single implant per tooth [Figure 6, Figure 22c].
Placement of implants and impression making
The oral cavity was rinsed with 1% Povidone Iodine mouth wash prior to the implant placement procedure. Local infiltration with 2% Lignocaine and 1:80000 Adr was done for mandibular procedures. However, for maxillary procedures, a nerve block along with local infiltration, akin to a dental extraction procedure was carried out. A straight surgical handpiece with a physio dispenser with 1:1 torque and 20000 rpm were used to drill the osteotomy. The path finder (pilot) drill was used in mandibular anterior region where the bone appeared to be very hard, however for all other sites the osteotomy was done using a 2mm (30/40mm) twist drill directly. The osteotomy depth and direction were decided intraop depending on the tactile feedback indicating penetration of the second / third cortical bone. Various principles of cortical engagement were used in order to firmly place the implants in the residual alveolar ridge. The implant heads were subsequently bent to achieve approximate parallelism using the insertion adapter and or ratchet. [Figure 2a,b, ] [Table 1]. No torque measuring device was used in our study, the firmness of the implant was determined empirically. Pickup impression was made after placement of the impression caps on the implants using addition silicone impression material on stock trays. In case of full mouth restorations or long span segments the impression caps were stabilized using light cure composite material [Figure 2c, Figure 3]
.
The occlusal reduction of the implants was then carried out for single tooth and segment cases in order to remove occlusal interferences, this however was not required to be done in full mouth rehabilitation cases. The patient was prescribed broad spectrum antibiotics as per the following regimen: Tab Amoxicillin + Clavulanic acid 1.2 gms BD, Tab Tinidazole 500 mg BD, Tab Ibuprofen 400 mg + Paracetamol 325 mg, Tab B Complex OD, and Tab Ranitidine 150 mg BD. An OPG was done to verify the implant placement [Figure 4, Figure 5, Figure 6 ].
Metal framework trial, bite registration & wax trial
Metal framework trial, bite registration and wax trial was done in full mouth rehabilitation and long span segment rehabilitation cases, however, for single tooth / short span cases the final prosthesis was seated directly [Figure 7, Figure 8 a,b].
During the metal framework trial in full mouth rehabilitation cases and prosthesis insertion for single tooth / segment, the implant heads were trimmed occlusally using a metal cutting bur on an airrotar handpiece. Care was taken not to reduce / alter the cervical 1/3rd (4mm) of the implant head while preparing it for metal framework trial/ prosthesis insertion. Once the metal framework was seated in the mouth, bite registration was done using modelling wax. Thereafter, the models were articulated, and teeth setup done. This setup was then tried in the patient mouth [Figure 8b]. On satisfactory completion of the wax trial the prosthesis was conventionally finalized. For FMR cases a metal acrylic (Hybrid) prosthesis was used, however for segment cases PFM prosthesis was constructed.
Prosthesis insertion & occlusal balancing
A hard and fast setting glass ionomer cement e.g. GC Fuji Plus, was used to cement the prosthesis. Removal of the excess cement was ensured after set. The occlusion was verified, and all lateral and protrusive contacts were eliminated in full mouth rehabilitation cases. A lingualized occlusion was established with occlusal contacts on the lingual aspect of the premolars and the first molar with cross arch balance. The patient was instructed to chew soft food and maintain oral hygiene.
Postoperative review
Post-operative OPG was done after final seating of the prosthesis in order to verify the fit of the prosthesis and presence of residual cement in the periphery of the implants or soft tissues. Post-operative review was done after 1 week, 3 months, 6 months, and 1 year. Thereafter, the patient was advised yearly review. An OPG was advised for the 6- and 12-month review.
Results
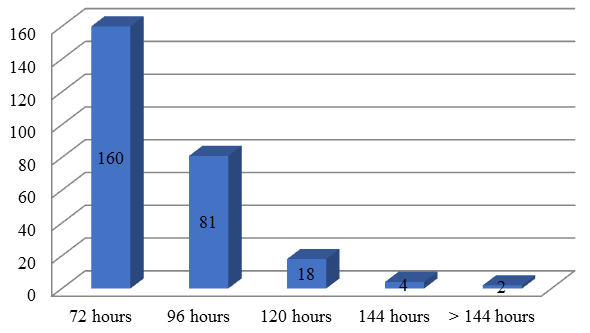
A total of 265 implants were placed over a period of one year. 247 implants were bent after placement [Table 1]. In our study 160 implants were loaded within 72 hours, 81 implants in 96 hours, 18 implants in 120 hrs, 04 implants in 144 hours and 02 implants were unloaded due to unavailability of the patient [Chart 1]. 06 implants failed and had to be removed from the patient’s mouth. 02 of the failed implants were unloaded due to unavailability of the patient. 04 of the failed implants became loose after 03 months of use and had to be removed [Table 2]. Other complication included 02 cases of acrylic teeth fracture [Table 3]. These were repaired using composite resins. Statistical analysis was carried out using SPSS 16.0. Welch T test was done to ascertain the survivability of different group of implants from 72 to 144 hrs. The P value was 0.1315 which by conventional criteria is statistically not significant.
Table 1
Bent vs unbent implants
| S. No | Number of implants | Bent/Unbent |
| 1. | 18 implants / Distal Pterygoid and maxillary anterior region | Unbent |
| 2. | 247 implants | Bent |
Table 2
- Implant failure cases
Discussion
The key result area for SCI is the rapidity with which the implant can be functionally loaded vis-à-vis the other contemporary implant techniques 6 and its effectiveness in various clinical scenarios without the need of undertaking any adjunctive procedures. This speed of immediate functional loading using the BECES implant however depends on several diagnostic inferences, operative plans and apt intermediate goals leading on to a successful final rehabilitation of an edentulous patient. Standard preoperative diagnostic protocols i.e. blood tests and optimization of systemic conditions are imperative to treatment planning. The radiological investigation of choice depends on the operator’s preference based on experience and understanding and on the specific requirements of the implant system and the case. Although in conventional implantology CBCT is the commonly advised investigation to gain the necessary diagnostic information, at our centre OPG is the investigation of choice for placement of SCI. This radiograph gives a two-dimensional image of the bone availability of desired area, along with other findings i.e. impacted / retained teeth or root stumps, cystic lesions, altered bone morphology, the anatomy of the condyle etc. The operator identifies the second / third corticals to be used to engage the implants, this in turn determines the size and length and type of SCI to be used. 12 It is important to carefully assess the radiograph in totality because the designated implant site may not be the final implant position as the implant during placement at this predetermined location may not generate enough torque, thus warranting minor shifting of the site by creating a new osteotomy in the first, second or third cortical bone. In conventional implantology CBCT is preferred as there is a need to ascertain the volume and type of cancellous bone available to place an implant safely by avoiding encroachment on critical structures like the IAN and the maxillary sinus. Since the SCI takes its primary anchorage from the second and or third cortical bone [Figure 12, Figure 13, Figure 18] and avoids the IAN by the bypass technique, CBCT does not provide any value addition to treatment planning and or placement of SCI. Based on the same premise the use of surgical guides becomes redundant. In our practice we do not advocate the use of surgical splints as it restricts the spatial orientation of the operator by curtailing the ability to use alternative sites to achieve anchorage of the implants as per the prescribed methods, in case the initially planned site does not produce sufficient torque. The SCI placement is guided by a set of consensus methods, which are reassessed and revised regularly by the consensus group.7 Of these methods, the ones we commonly use in our cases are as follows: 1a - Multidirectional implant placement [Figure 4], 1b – Strategic implant placement with addition of stabilizing implants [Figure 4], 1c – Anchorage of implants in second / third cortical, independent of alveolar bone, preferably in resorption stable bone. [Figure 4],
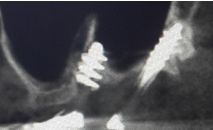
2. Mandibular anterior implants - Chin area placement, between the mental foramen, with or without necessity of engaging the second cortical [Figure 11], 3. Anchorage of a segment bridge with a long strategic implant between the mental nerve and the canine root [Figure 12], 4. Nerve bypass – buccal / lingual [Figure 13]
5a. Lingual cortical engagement in the distal mandible [Figure 13 ], 5b. Vestibular cortical engagement [Figure 13], 6. Placement of a wide diameter implant using the buccal and lingual/palatal corticals without anchorage of the second cortical [Figure 14], 7a. Anchorage of implants in the floor of the nose [Figure 13], 7b. Palatal insertion of the implant in the nasal floor bypassing the alveolar bone [Figure 15] 11, 8a - Placement of the apical threads of the implant in the cortical floor of the maxillary sinus [Figure 16], 8b - Use of intrasinusal buttress for multiside cortical engagement [Figure 17] 11, 9. Upper canine bypass [Figure 18],
10. Placement of implant in pterygoid bone [Figure 10], 10a - Double tubro-pterygoid [Figure 10], 11a - Anchorage in the bone palatal to the maxillary sinus without anchorage in the floor of the nose or mid palatine raphe[Figure 16], 11b – with anchorage in the floor of the nose or mid palatine raphe[Figure 14], 12. Placement of BECES implant in the zygomatic bone[Figure 19].
In our practice we use the polished surface bendable immediate functional loading strategic corticobasal BECES implant for the management of all types of edentulous cases based on the following premise 1. The incidence of peri-implantititis is lower than the rough surface implants 5. 2. The bendability of the polished surface is easier and to a greater extent as compared to a rough surface or hybrid implant which makes them easier to place and gives them better survivability due to better load distribution.6, 7 The use of SCI obviates the need for adjunctive procedures like sinus lift, bone grafting etc 7. 3. The elasticity of these implants provides resistance to dislodgement of the prosthesis as these are imperfectly parallel at insertion stage, thus providing resistance to dislodgement. 4. These are true cortical implants and are placed in the resorption stable second / third cortical bone vis-à-vis the rough surface implants which are placed in resorption prone cancellous bone. The polished surface implants owe their success to the fact that they derive primary anchorage from a site which is remote from the area which is most commonly prone to infection / periimplantitis i.e. the area which emerges out of the mucosa. Additionally, the soft tissue implant interface is on polished titanium thus avoiding peri-implant infection due to good biocompatibility. The bendability of these implants gives it the unique ability to safely avoid the only critical structure in the mandible i.e. the IAN. This is done using the buccal and lingual bypass technique, wherein the implant is anchored bucco-inferior or linguo-inferior to the nerve [Figure 13]. Buccally it derives anchorage from the cortical bone of the buccal shelf and lingually from the mylohyoid ridge. In the maxilla there are no critical structural limitations akin to the mandible. Unlike the rough surface crestal implantology, while using polished surface bendable implants, the floor of the maxillary sinus can be used to anchor the implant [Figure 16, Figure 17, Figure 18]. Trans-sinus placement of these implants is commonly done to engage the third cortical i.e. in the nasal floor, nasomaxillary buttress, pterygoid bone and or the zygomatic bone with no adverse clinical outcomes [Figure 14, Figure 16, Figure 19]. After placing the implants, it has been recommended to functionally load them with in 72 hrs in order to avoid failure by virtue of loading the implant when the bone is undergoing osteoclastic changes 7. However, our study could not strictly adhere to this recommendation. The delay in loading was not deliberately selective as it was a result of unavailability of the patients due to personal exigency and in very few cases due to delay in lab work. Fortunately, the clinical outcome was not affected significantly except in two cases where the implants failed because the patients reported back after two - three weeks of placement for loading, by which time the implants were infected and mobile. There is however a need to assess this in much greater detail to ascertain the limits of allowable time lapse in different clinical scenarios.
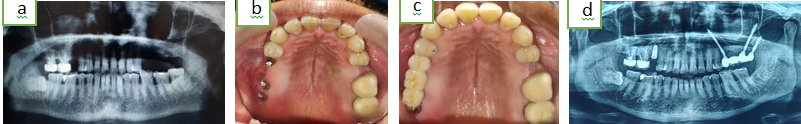
Since there is sparse commonality between the type of implant used / protocol & methodology in our study and that used for crestal / rough surface conventional implants, a comparative study of these two treatment modalities does not seem to be feasible. However, standard meta-analysis and other published data can be compared to assess the outcome of SCI versus the crestal implantology. We have reported a high success / survival rate of 97.7% with SCI, which is at par with the best reported data 12. Additionally, we report no requirement of any bone augmentation procedure like, sinus lift, bone grafting, alveolar bone distraction, ridge split, socket shield, pontic shield etc in our study which is a definite advantage over the conventional implantology as the later requires a large number of adjunctive procedures. We also advocate the use of metal acrylic hybrid circular dentures for its adaptability due to lower wear resistance and repairability as compared to the harder ceramic bridges [Figure 20 a-g] (Full mouth rehabilitation). However, ceramic / ceramic fused to metal bridges are recommended for single tooth or segment rehabilitations.[Figure 21 a-d] (Upper segment rehabilitation), [Figure 22a-d] (Lower segment rehabilitation), [Figure 23a-d] (Lower single tooth replacement), [Figure 24 a-d] (Upper single tooth replacement)]
The failures we have encountered were ascribed to underloading / overloading of the implants which were readily rectified using correct / timely prosthesis placement and or placing adequate number of implants. Other complications included fracture of the acrylic teeth which was repaired using composite resin [Figure 25 a, b, c].
Conclusion
In our study we observed that the versatility of the strategic corticobasal BECES implant is unmatched with regards to speed of rehabilitation and complete obviation of the need for adjunctive procedures like sinus lift, bone grafting etc. The function and aesthetics are at par with the best published data in dental implantology with survivability rate higher than any other. In our practice the OPG seems to suffice our requirements in majority of our cases both for preoperative planning and postoperative review and the requirement of a CBCT has been minimal. In our observation the consensus group recommendation of 72-hour loading window after implant placement does not appear to be very sacrosanct. A much larger and longer study assessing this aspect in greater detail is warranted as this has a bearing on the stress it places on the operator and the dental laboratory to meet the recommended deadline. In order to successfully and satisfactorily practice this art and science, there is a need to correctly learn this methodology as its concepts are tangential to those of the currently more popular crestal rough surface implantology. The surgical and prosthodontic acumen and understanding of the operator must be thorough to be able to harness the complete potential of these implants to deliver a long term reliable rehabilitative solution for any given edentulous situation. Inferring Professor Paul Stoelinga’s words “Techniques and devices are presented as a revolution in the specialty, as if the previous techniques were obsolete and not worth using. As the novelty element fades away, the basic rules of surgery always prevail whereas the techniques and revolutionary devices turn into a step of the field’s evolution” 13, at the moment, the principles and practice of strategic corticobasal implantology may appear to be at a novel tangent to the more prevalent practices of the day, however, it may not be long, before the SCI blends in with our overall efforts towards better patient care.