Introduction
Biomaterials research has progressed steadily in the past few decades and is leading to an improvement in human life expectancy. Dental work includes changing existing materials or designing new and improved products for prosthetic applications. Dentures made of PMMA were popular because of their ability to be molded with ease, excellent esthetics and satisfactory mechanical properties. An ideal denture base material is the one that possesses biocompatibility, excellent esthetics, superior mechanical properties especially modulus of elasticity, impact strength, flexural strength and hardness, sufficient bond strength with artificial teeth, ability to repair and dimensional accuracy. 12
Poly methyl methacrylate is as yet the most overwhelmingly utilized denture, but, it has certain drawbacks like thermal shrinkage, poor mechanical and fatigue strength, brittle on impact, poor color stability of self-cured resins, residual monomer allergy, porosity, poor conductors of heat and requirement of mechanical retention.34 Plenty of research literature is available on denture base resins and considering their inherent drawbacks, several researches have been conducted to improve their physical and mechanical properties by reinforcing with various materials. So, this review article aims at compiling different materials from articles published through the years 1971 to 2017.
The use of hypoallergenic resins overcame the issues of monomer allergy. Therapeutic use of thermoplastic resins has increased. 34 Smith (1957) reported on glass reinforcement of PMMA by mixing discrete fibres with the dough or by lamination with glass cloth. Jennings & Wuebbenhorst (1960) reported on the reinforcement of pedodontic prosthetic appliances with stainless steel mesh, braided wire plate, a stainless steel lingual bar and stainless steel wire. Schreiber (1971), in a preliminary report on the reinforcement of PMMA with carbon fibres, discussed the use of acrylic resin composite prepegs. Bucknall (1977) discussed the addition of rubbers to PMMA. Bowman & Manley (1984) confirmed that the reinforcement of upper dentures with carbon fibre/PMMA inserts significantly reduced the number of breakages. Fraunhofer (1984) determined the effect of reinforcing autopolymerizing acrylic resin with flat braided two strand brass wire and orthodontic wire. Vallittu & Narva (1997) reported a composite that consists of glass fibres and aramid fibres reinforced in resin matrix.5
Classification
Denture base reinforcing materials are broadly classified into: Non-metals and Metals.
A. Non- Metals
1. Rubber reinforced PMMA2O3)- Zirconia (ZnO2)- Silica (SiO2)- Nanodiamond- Carbon- Halloysiteii. Nanofibers- Glass nanofibers- HA- Polyacrylonitrile and PMMA nanofibersB. Metals1. Metal fiber reinforced resins2. Metal insertsi. Stainless Steel wiresii. Brass wires3. Nanofillersi. Silverii. Copperiii. Titanium (TiO2)iv. Goldv. Platinumvi. Palladium
Rubber Reinforced Poly Methyl Methacrylate (PMMA
Sufficient impact strength and fracture toughness are most essential for denture base resins. One of the main drawbacks of PMMA denture bases is low fracture toughness. Many studies have been performed to evaluate the toughness and mechanisms of toughness improvement in rubber-modified acrylic polymers. 67 In these polymers, the resin matrix is filled with a rubbery particle which has a modulus of elasticity lower than that of the polymer matrix. Therefore the reinforced polymer will have a lower modulus compared to the unmodified polymer. The most significant advantage of this modification is an increase in toughness and ultimate elongation in comparison with the relatively brittle resin acrylic material.8
High Impact Resins
Rubber reinforced (butadiene-styrene polymethyl methacrylate) particles grafted to MMA for improved bond with PMMA. They have greater impact strength & fatigue properties and so, they are indicated for patients who drop their dentures repeatedly e.g. parkinsonism. Available as powder-liquid system & processing is samilar to heat-cure resins.
Fiber Reinforced Resins
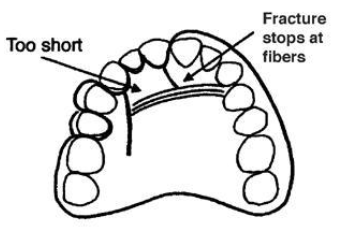
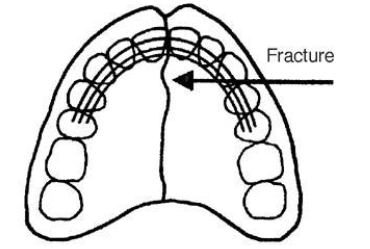
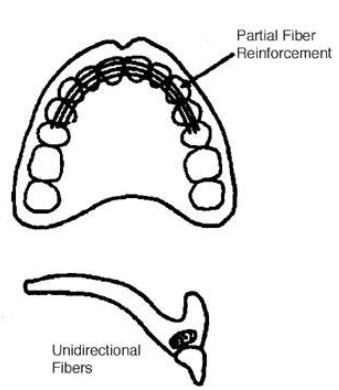
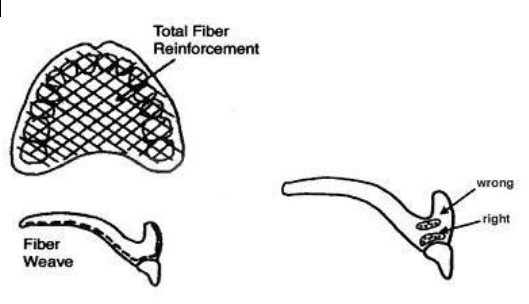
Poor impact strength and poor fatigue resistance is primary issue with PMMA. A research by Johnston et al. reveals that within a few years of manufacture 68 percent dentures break. Mostly they are due to a combination of fatigue and impact. Fiber reinforcement leads to an improvement in strength.
Table 1
Hypoallergenic Resins
Addition of hydroxyapatite fillers increases fracture toughness. 25 Addition of Al2O3 fillers increases the flexural strength & thermal diffusivity that could lead to more patient satisfaction. 26 The ratio of 2.2:1 by weight of powder to liquid was found to be the best ratio for mixing the material to give the best results in formulation. 27 28 Addition of ceramic or sapphire whiskers to improve thermal diffusivity. 29 Addition of 11-14% of several compounds of either bismuth or uranium or 35% of an organo-zirconium compound impart radiopacity equivalent to that of aluminium. 30 Addition of Triphenyl Bismuth (Ph3Bi) is a promising new additive to provide radiopacity. 31
Thermoplastic Resins
This new procedure, during which a fully polymerized basic material is softened by heat and injected afterwards, has opened up a new chapter in making dentures. 31
Advantages
They provide excellent esthetics with tooth or tissue colored materials and are very comfortable for the patient. These are stable, have high fatigue endurance, high creep resistance, excellent wear characteristics & solvent resistance. They are non-porous so no growth of bacteria, and even if it is non-porous, it still retains a slight amount of moisture to keep it comfortable against gums. They are unbreakable, flexible, light weight and have very little or no monomer content. 31
Thermoplastic nylon
The principal constituent of thermoplastic nylon is polyamide. It uses Rapid Injection which introduced the first flexite thermoplastic. Thermoplastic nylon is injected at temperatures from 274 to 293oC. This material generally replaces the metal, and the pink acrylic denture material used to build the framework for standard removable partial dentures. 32 Valplast & flexiplast are polyamides (nylon plastics), since then there is a continued interest in thermoplastic dental materials.33, 34
Advantages
It is virtually invisible (translucent allowing natural tissue to show through), and there are no metal clasps, only tissue coloured clasps that blend with natural teeth, thus provides excellent esthetics.34, 35, 36, 37, 38 Nylon is unbreakable, light weight & does not warp or become brittle. Because of its flexibility & incredible patient comfort, nylon is ideal for patients considering a removable partial denture. In addition, it involves non-invasive procedures & can be relined or repaired. Nylon shows no discoloration over time & is non-porous so no growth of bacteria. 34, 35, 36, 37, 38
Limitations
Nylon is little more difficult to trim & polish. Also it is not strong enough for conventional tooth borne rest seats. 34
Thermoplastic acetal
Acetal was first proposed as an unbreakable thermoplastic resin removable partial denture material in 1971. Rapid injection system developed the first tooth coloured clasps with thermoplastic fluoropolymer.39 In 1986, Dental ‘D’ reintroduced tooth colored clasps using Acetal resin. Acetal as a homo-polymer has good short-term mechanical properties, but as a co-polymer has better long-term stability.
Table 2
Mechanism of action
Resin clasps engage the first third (or origin) of the undercut rather than the terminal third as in metal clasps allowing three to four times the retention of metal. The clasp can then be placed more gingival increasing its aesthetic appeal beyond the obvious colored properties.42
Adavntages
Thermoplastic acetal comes in 18 Vita shades + 3 pink shades, to match most people’s teeth or gums and clasps are tooth coloured clasps so provide good esthetics. Labial bars can replace bulky, un-aesthetic metal swing-lock type bars. Acetal is flexible and hypoallergenic (monomer free). The teeth and clasps can be injected together in resin, or into the existing denture adding many new applications. Adjusting is usually not necessary. 39
Limitations
An injected resin major connector for temporary partials is no longer recommended because the major connectors must be rigid while resin is flexible and moreover it will not seal around the base of denture teeth allowing seepage of fluid under and around the teeth. Their use is limited in resin anterior teeth because it does not have the natural translucency. 39
Applications
Acetal resin is very strong, resists wear and fracturing, and is quite flexible. These characteristics make it an ideal material for pre-formed clasps for partial dentures, single pressed unilateral partial dentures, partial denture frameworks, provisional bridges, occlusal splints, and even implant abutments.49
Thermoplastic acrylic
Heat-cure PMMA shows high water absorption, volumetric changes and residual monomer and porosity.50 Even though Thermoplastic acrylic has poor impact resistance, it has enough tensile and flexural strength. It is available in tooth and gingival colors and has good esthetics. Acrylic doesn't wear as much during occlusal forces and consequently won't maintain vertical dimension over long periods of your time. 50
Thermoplastic polycarbonate
It is a polymer chain of bisphenol-A carbonate. It is similar to Acetal resin, and is also strong, resists fracture, is flexible and does not wear. Polycarbonate is used for temporary crown & bridges. The material has a good translucency and finishes very well, providing improved esthetics. 39, 49, 50
Advantages
It doesn’t use monomer and a catalyst in process so residual monomer doesn’t begin to melt. It also has lesser water sorption property and so, no offensive odour and does not cause redness of oral mucous membrane. 39, 49, 50
Disadvantages
Complicated processing equipments with greater distortion from water sorption, high flexibility, low adhesion to acrylic teeth and low hardness.
Applications of thermoplastic resins
Applications of thermoplastic resins include:
Implant abutments
Preformed partial denture clasp,
Flexible tooth born partial denture framework,
Occlusal appliances,
Orthodontic and sleep apnea appliances.
Provisional crowns and bridges,
Single cast partial dentures 51
Nanomaterials
The concept of nanotechnology was first introduced in 1959 by Feynman. Since then, nanotechnology has been widely used in many applications, including medical sciences, and plays an important role in diagnosis, treatment, and regenerative medicine.52 A nanomaterial is an object, which at least one of its dimensions is at the nanometer scale (approximately 1 to 100 nm). Nanomaterials are categorized according to dimension – those with all 3 dimensions less than 100 nm [nanoparticles (Nps)]; those that have 2 dimensions less than 100 nm (nanotubes, nanofibers, and nanowires); and those that have one dimension less than 100 nm (thin films, layers, and coatings).53 Use of nanomaterials in composites have achieved better esthetics and mechanical properties. 54
Nanofillers
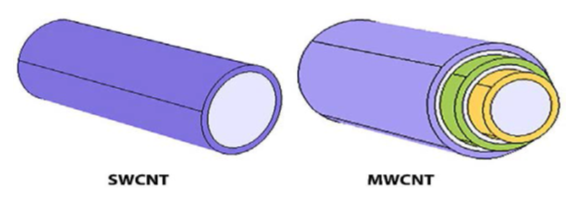
Size, shape, surface area, concentration, and dispersion of nanofillers into resin matrix all affect its mechanical properties. Alumina NPs, zirconia (ZrO2) NPs, titania (TiO2) NPs, silver NPs, gold NPs, Pt NPs, HA NPs, SiO2 NPs etc are introduced to improve the mechanical properties of PMMA. 13 Nanofillers are available in different shapes such as cones, spheres, rods, tubes and flowers. Carbon nanotubes (CNTs), ZrO2 nanotubes, TiO2 nanotubes, and halloysite nanotubes (HNT) are among the nanotubes used for reinforcement of dental materials. CNTs are classified into 2 main types according to the structure of the CNTs– single-walled and multi-walled (Figure 7).55
Self Reinforcement
Self-reinforced materials have been used in polyglycolic acid resorbable screws and plates and collagen forming materials. Gilbert, Ney & Lautenschlager in 1995, has discussed this concept of self-reinforcement of polymers. The concept is based on the idea of a fibrous material, which is chemically identical to the matrix holding the fibres in place. The composite material consisted of high strength, high ductility PMMA fibres embedded in a matrix of PMMA. The properties of unidirectional continuous form were evaluated and showed significantly greater tensile properties, flexural ductility, fracture toughness and fatigue strength compared with bulk PMMA. 5
Conclusion
The progress in denture base resins have provided encouraging results pertaining to its strength and esthetics. Many drawbacks of PMMA denture base resins have been conqured and it is certain that in future, research will offer newer materials which are more biocompatible with better mechanical endurance, offering better treatment and care to the patient.